Compositions and methods for treating cancer with anti-CD 33 immunotherapy
阅读说明:本技术 用于用抗cd33免疫疗法治疗癌症的组合物和方法 (Compositions and methods for treating cancer with anti-CD 33 immunotherapy ) 是由 迪米特尔·S·迪米特罗夫 里马斯·奥伦塔什 迪娜·施奈德 博罗·德罗普利奇 朱忠玉 于 2018-03-23 设计创作,主要内容包括:本发明涉及用于用抗CD33免疫疗法治疗癌症的组合物和方法。本公开内容涉及包含CD33抗原结合结构域的嵌合抗原受体(CAR),包括核酸、重组表达载体、宿主细胞、抗原结合片段和药物组合物。还公开了在对象中治疗或预防癌症的方法和制备嵌合抗原受体T细胞的方法。提供了与来源于人CD8蛋白的跨膜结构域、4-1BB共刺激结构域和CD3ζ信号转导结构域偶联的7种不同CD33外部结构域的实验结果。(The present invention relates to compositions and methods for treating cancer with anti-CD 33 immunotherapy. The present disclosure relates to Chimeric Antigen Receptors (CARs) comprising a CD33 antigen binding domain, including nucleic acids, recombinant expression vectors, host cells, antigen binding fragments, and pharmaceutical compositions. Also disclosed are methods of treating or preventing cancer in a subject and methods of making chimeric antigen receptor T cells. Experimental results are provided for 7 different CD33 outer domains coupled to a transmembrane domain derived from human CD8 protein, a 4-1BB costimulatory domain, and a CD3 zeta signaling domain.)
1. An isolated nucleic acid molecule encoding a Chimeric Antigen Receptor (CAR) comprising at least one extracellular antigen-binding domain comprising a CD33 antigen-binding domain encoded by a nucleotide sequence comprising SEQ ID No.1, 3, 5,7, 9, or 11, at least one transmembrane domain, and at least one intracellular signaling domain.
2. The isolated nucleic acid molecule of claim 1, wherein the encoded at least one CD33 antigen binding domain comprises at least one single chain variable fragment of an antibody that binds to CD 33.
3. The isolated nucleic acid molecule of claim 1, wherein the encoded at least one CD33 antigen binding domain comprises at least one heavy chain variable region of an antibody that binds to CD 33.
4. The isolated nucleic acid molecule of claim 1, wherein the encoded at least one CD33 antigen binding domain, the at least one intracellular signaling domain, or both are linked to the transmembrane domain by a linker or spacer domain.
5. The isolated nucleic acid molecule of claim 4, wherein the encoded linker or spacer domain is derived from the extracellular domain of CD8, TNFRSF19, or CD28 and is linked to the transmembrane domain.
6. The isolated nucleic acid molecule of claim 1, wherein the encoded extracellular CD33 antigen-binding domain is preceded by a leader nucleotide sequence encoding a leader peptide.
7. The isolated nucleic acid molecule of claim 6, wherein the leader nucleotide sequence comprises a nucleotide sequence comprising: encoding the amino acid sequence of SEQ ID NO: 14, SEQ ID NO: 13, or encodes SEQ ID NO: 40 of the leader amino acid sequence of SEQ ID NO: 39, or encodes SEQ ID NO: 42 of the leader amino acid sequence of SEQ ID NO: 41, or encodes SEQ ID NO: 44 of the leader amino acid sequence of SEQ ID NO: 43.
8. the isolated nucleic acid molecule of claim 1, wherein the transmembrane domain comprises a transmembrane domain of a protein comprising: an α, β, or ζ chain of a T cell receptor, CD8, CD28, CD3 ∈, CD45, CD4, CD5, CD8, CD9, CD16, CD22, CD33, CD37, CD64, CD80, CD83, CD86, CD134, CD137, CD154, and TNFRSF19, or any combination thereof.
9. The isolated nucleic acid molecule of claim 1, wherein the nucleic acid sequence encoding the extracellular CD33 antigen binding domain comprises a nucleotide sequence comprising SEQ ID NO: 1. 3, 5,7, 9 or 11, or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto.
10. The isolated nucleic acid molecule of claim 1, wherein the encoded at least one intracellular signaling domain further comprises a CD3 ζ intracellular domain.
11. The isolated nucleic acid molecule of claim 10, wherein the encoded at least one intracellular signaling domain is disposed on the C-terminal side relative to the CD3 ζ intracellular domain.
12. The isolated nucleic acid molecule of claim 1, wherein the encoded at least one intracellular signaling domain comprises a co-stimulatory domain, a primary signaling domain, or any combination thereof.
13. The isolated nucleic acid molecule of claim 12, wherein the encoded at least one co-stimulatory domain comprises a functional signaling domain of OX40, CD70, CD27, CD28, CD5, ICAM-1, LFA-1(CD11a/CD18), ICOS (CD278), DAP10, DAP12, and 4-1BB (CD137), or any combination thereof.
14. A Chimeric Antigen Receptor (CAR) encoded by the isolated nucleic acid molecule of claim 1.
15. The CAR of claim 14, comprising at least one extracellular antigen-binding domain comprising a CD33 antigen-binding domain comprising the amino acid sequence of SEQ ID No.2, 4,6, 8, 10, or 12, at least one transmembrane domain, and at least one intracellular signaling domain.
16. The CAR of claim 15, wherein the CD33 antigen binding domain comprises at least one single chain variable fragment of an antibody that binds to CD 33.
17. The CAR of claim 15, wherein the CD33 antigen binding domain comprises at least one heavy chain variable region of an antibody that binds to CD 33.
18. The CAR of claim 15, wherein the transmembrane domain comprises a transmembrane domain of a protein comprising: an α, β, or zeta chain of a T cell receptor, CD8, CD28, CD3 epsilon, CD45, CD4, CD5, CD8, CD9, CD16, CD22, CD33, CD37, CD64, CD80, CD86, CD134, CD137, CD154, and TNFRSF19, or any combination thereof.
19. The CAR of claim 18, wherein the CD8 transmembrane domain comprises the amino acid sequence of SEQ ID NO: 27, or an amino acid sequence that is identical to SEQ ID NO: 28, has an amino acid sequence of 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity.
20. The CAR of claim 15, wherein the at least one extracellular antigen-binding domain and the at least one intracellular signaling domain, or both, are linked to the transmembrane domain by a linker or spacer domain, the extracellular antigen-binding domain comprising a CD33 antigen-binding domain comprising the amino acid sequence of SEQ ID No.2, 4,6, 8, 10, or 12.
21. The CAR of claim 20, wherein the linker or spacer domain is derived from the extracellular domain of CD8, TNFRSF19, IgG4, or CD28 and is linked to the transmembrane domain.
22. The CAR of claim 17, wherein the at least one intracellular signaling domain comprises a costimulatory domain and a primary signaling domain.
23. The CAR of claim 22, wherein the at least one intracellular signaling domain comprises a co-stimulatory domain comprising a functional signaling domain of a protein selected from the group consisting of: OX40, CD70, CD27, CD28, CD5, ICAM-1, LFA-1(CD11a/CD18), ICOS (CD278), DAP10, DAP12, and 4-1BB (CD137), or any combination thereof.
24. A vector comprising the nucleic acid molecule of claim 1.
25. The vector of claim 24, wherein the vector is selected from the group consisting of: a DNA vector, an RNA vector, a plasmid vector, a cosmid vector, a herpes virus vector, a measles virus vector, a lentiviral vector, an adenoviral vector, or a retroviral vector, or a combination thereof.
26. The vector of claim 24, further comprising a promoter.
27. The vector of claim 26, wherein the promoter is an inducible promoter, a constitutive promoter, a tissue specific promoter, a suicide type promoter, or any combination thereof.
28. A cell comprising the vector of claim 24.
29. The cell of claim 28, wherein the cell is a T cell.
30. The cell of claim 28, wherein the T cell is CD8+T cells.
31. The cell of claim 28, wherein the cell is a human cell.
32. A method of making a cell comprising transducing a T cell with the vector of claim 24.
33. A method of producing a population of RNA-engineered cells comprising introducing in vitro transcribed RNA or synthetic RNA into a cell, wherein the RNA comprises the nucleic acid molecule of claim 1.
34. A method of providing anti-tumor immunity in a mammal, comprising administering to the mammal an effective amount of the cell of claim 28.
35. A method of treating or preventing cancer in a mammal comprising administering to the mammal the CAR of claim 15 in an amount effective to treat or prevent cancer in the mammal.
36. A pharmaceutical composition comprising an anti-tumor effective amount of a population of human T cells, wherein the T cells comprise a nucleic acid sequence encoding a Chimeric Antigen Receptor (CAR), wherein the CAR comprises at least one extracellular antigen-binding domain comprising a CD33 antigen-binding domain comprising the amino acid sequence of SEQ ID No.2, 4,6, 8, 10, or 12, at least one linker domain, at least one transmembrane domain, at least one intracellular signaling domain, and wherein the T cells are T cells of a human having cancer.
37. The pharmaceutical composition of claim 36, wherein the at least one transmembrane domain comprises a transmembrane domain of a protein comprising: an α, β, or zeta chain of a T cell receptor, CD8, CD28, CD3 epsilon, CD45, CD4, CD5, CD8, CD9, CD16, CD22, CD33, CD37, CD64, CD80, CD86, CD134, CD137, and CD154, or any combination thereof.
38. The pharmaceutical composition of claim 36, wherein the T cell is a T cell of a human having a hematologic cancer.
39. The pharmaceutical composition of claim 38, wherein the hematologic cancer is leukemia or lymphoma.
40. The pharmaceutical composition of claim 39, wherein the leukemia is Acute Myeloid Leukemia (AML), blastic plasmacytoid dendritic cell tumor (BPDCN), Chronic Myeloid Leukemia (CML), Chronic Lymphocytic Leukemia (CLL), acute lymphocytic T cell leukemia (T-ALL), or acute lymphocytic B cell leukemia (B-ALL).
41. The pharmaceutical composition of claim 39, wherein the lymphoma is mantle cell lymphoma, non-Hodgkin's lymphoma, or Hodgkin's lymphoma.
42. The pharmaceutical composition of claim 38, wherein the hematologic cancer is multiple myeloma.
43. The pharmaceutical composition of claim 36, wherein the human cancer comprises adult cancer including oral and pharyngeal cancer (tongue, mouth, pharynx, head and neck), digestive system cancer (esophagus, stomach, small intestine, colon, rectum, anus, liver, intrahepatic bile duct, gallbladder, pancreas), respiratory system cancer (larynx, lung and bronchi), bone and joint cancer, soft tissue cancer, skin cancer (melanoma, basal cell and squamous cell carcinoma), pediatric tumors (neuroblastoma, rhabdomyosarcoma, osteosarcoma, ewing's sarcoma), tumors of the central nervous system (brain, astrocytoma, glioblastoma, glioma), and breast, reproductive system (cervix, uterus, ovary, vulva, vagina, prostate, testis, penis, endometrium), urinary system (bladder, kidney and renal pelvis, ureter), eye and orbital, and cervical cancer, Cancer of the endocrine system (thyroid), and of the brain and other nervous systems, or any combination thereof.
44. A method of treating a mammal having a disease, disorder or condition associated with elevated expression of a tumor antigen, the method comprising administering to a subject a pharmaceutical composition comprising an anti-tumor effective amount of a population of T cells, wherein the T cells comprise a nucleic acid sequence encoding a Chimeric Antigen Receptor (CAR), wherein the CAR comprises at least one extracellular antigen-binding domain comprising a CD33 antigen-binding domain comprising the amino acid sequence of SEQ ID No.2, 4,6, 8, 10 or 12, at least one transmembrane domain, at least one intracellular signaling domain, wherein the T cells are T cells of a subject having cancer.
45. A method of treating cancer in a subject in need thereof, the method comprising administering to the subject a pharmaceutical composition comprising an anti-tumor effective amount of a population of T cells, wherein the T cells comprise a nucleic acid sequence encoding a Chimeric Antigen Receptor (CAR), wherein the CAR comprises at least one extracellular antigen binding domain comprising a CD33 antigen binding domain comprising the amino acid sequence of SEQ ID No.2, 4,6, 8, 10, or 12, at least one linker or spacer domain, at least one transmembrane domain, at least one intracellular signaling domain, wherein the T cells are T cells of a subject having cancer.
46. The method of claim 44 or 45, wherein the at least one transmembrane domain comprises a transmembrane domain of a protein comprising: an α, β, or zeta chain of a T cell receptor, CD8, CD28, CD3 epsilon, CD45, CD4, CD5, CD8, CD9, CD16, CD22, CD33, CD37, CD64, CD80, CD86, CD134, CD137, and CD154, or any combination thereof.
47. A method for producing a cell expressing a chimeric antigen receptor, the method comprising introducing into a cell the isolated nucleic acid of claim 1.
48. The method for producing a cell expressing a chimeric antigen receptor according to claim 47, wherein the cell is a T cell or a population of cells comprising a T cell.
Technical Field
The present application relates to the field of cancer, and in particular to CD33 antigen binding domains and Chimeric Antigen Receptors (CARs) comprising such CD33 antigen binding domains and methods of use thereof.
Background
Cancer is one of the most fatal threats to human health. In the united states alone, cancer affects nearly 130 million new patients per year and is the second leading cause of death following cardiovascular disease, causing about one-fourth of deaths. Solid tumors are responsible for most of these deaths. Despite significant advances in the medical treatment of certain cancers, the overall 5-year survival rate of all cancers has only improved by about 10% over the past 20 years. Cancer or malignant tumors metastasize and grow rapidly in an uncontrolled manner, making treatment extremely difficult.
CD33 is a 67kDa transmembrane cell surface glycoprotein receptor. CD33 is a member of the sialic acid-binding immunoglobulin-like lectin (SIGLEC) family. Proteins in this family mediate leukocyte adhesion to endothelial cells by binding sialylated glycans. (Kelm S, Schauer R, Crocker PR. Glycoconj J. 1996; 13: 913. 926). In addition, CD33 acts as an inhibitory receptor through immunoreceptor tyrosine-based inhibitory motifs (ITIMs). Activation of the CD33 receptor leads to phosphorylation of two tyrosines (Y340 and Y358) in the cytoplasmic tail of CD33, which is the docking site for SHP phosphatase, and is involved in inhibitory signaling cascades, such as down-regulation of calcium mobilization (Paul SP1, Taylor LS, Stansbury EK, McVicar DW blood.2000 Jul 15; 96 (2): 483-90).
CD33 is a myeloid differentiation antigen and is highly expressed on myeloid progenitor cells (Andrews RG, Torok-Storb B, Bernstein ID. blood. 1983; 62: 124-. In contrast, CD33 has been reported to be expressed in 87.8% -99% of Acute Myeloid Leukemia (AML) (A Ehninger1 et al, Blood Cancer Journal (2014)4, e 218; Christina Krupka et al, Blood 2014123: 356-. AML is a devastating disease with a 5-year survival rate of about 26% (available on the world wide web, net/cancer-types/leukemia-acetic-muscle-AML/statics). The current standard of care for AML consists of: remission induction therapy by high dose chemotherapy or radiation followed by consolidation, including allogeneic stem cell transplantation and additional chemotherapy procedures as needed (available in world wide web cancer/access-muscle-leukemia/treatment/systemic-treatment-of-am. ht ml). The high toxicity associated with this treatment and the risk of complications (e.g., myelosuppression or GVHD) have prompted the search for better treatment options.
A number of new approaches to AML treatment are currently being investigated, including antibody-drug conjugates (SGN-CD33A, Vadastuximab Talirine, Stein A.S. et al, (2015). Blood, 126(23), 324; Phase I-II clinical trial NCT02706899), bispecific T cell adaptor antibodies (AMG330, Laszlo GS et al, Blood 2013: 123 (4): 554) 561, NCT02520427) and CART-33 cells (Wang QS et al, Mol der.2015 Jan; 23 (1): 184-91, NCT 01864902). However, due to clinical toxicity, a number of new approaches have been set aside. The Seattle Genetics Phase I Clinical trial (Seattle Genetics Phase I Clinical trials) testing SGN-CD33 drugs has recently been on the shelf due to the risk of hepatotoxicity (available on the world Wide Web business wire. com/news/home/20161227005087/en/Seattle-Genetics-innounc-Clinical-Hold-Phase-1). After observing the development of potentially fatal venous obstructive liver disease in a post-marketing clinical trial, manufacturers voluntarily withdrawn Gemtuzumab ozogamicin (Mylotarg, Pfizer/Wyeth) from the market in 2010 (Jacob mBlood 2013121: 4838-4841). Although the FDA recently reintroduced Mylotarg for CD33+ adult AML and relapsed/refractory pediatric AML, new, more conservative lower doses and new regimens were prescribed for this drug (FDA press release 2017, available on the world wide web FDA. gov). The efficacy of this treatment, the persistence of the patient's response to Mylotarg, the instances of tumor antigen escape and their safety profile under the new regimen remain to be determined. Therefore, there is an urgent need for safe, effective and durable treatments for AML.
Chimeric Antigen Receptors (CARs) are hybrid molecules comprising three basic units: (1) an extracellular antigen binding motif, (2) a ligation/transmembrane motif, and (3) an intracellular T cell signaling motif (Long AH, Haso WM, Orientas RJ. Lessons left from a high-active CD22-specific molecular antigen receptor. on immune.2013; 2 (4): e 23621). The antigen binding motif of a CAR is typically composed of a single chain variable Fragment (ScFv): the minimal binding domain of immunoglobulin (Ig) molecules is formed. Alternative antigen binding motifs, such as receptor ligands (i.e., IL-13 has been engineered to bind to tumor-expressed IL-13 receptors), whole immune receptors, library-derived peptides, and innate immune system effector molecules (e.g., NKG2D) have also been engineered. Alternative cellular targets for CAR expression (e.g., NK or γ - δ T cells) are also under development (Brown CE et al, Clin Cancer Res.2012; 18 (8): 2199-209; Lehner M et al, PLoS one.2012; 7 (2): e 31210). There is still a great deal of work on defining the most active T cell population to transduce using CAR vectors, determining the optimal culture and expansion techniques, and defining the molecular details of the CAR protein structure itself.
The linking motif of the CAR can be a relatively stable domain (e.g., the constant domain of IgG) or a flexible linker designed to extend. Structural motifs such as those derived from IgG constant domains can be used to extend ScFv binding domains away from the T cell plasma membrane surface. This may be important for some tumor targets where the binding domain is in particular close to the surface membrane of the tumor cell (e.g. for disialoganglioside GD 2; orantas et al, unpublished observations). To date, the signaling motif for CARs generally comprises the CD 3-zeta chain, as this core motif is a key signal for T cell activation. The first reported second generation CARs were characterized by a CD28 signaling domain and a CD28 transmembrane sequence. This motif is also used for third generation CARs that contain a CD137(4-1BB) signaling motif (Zhao Y et al, J immunol. 2009; 183 (9): 5563-74). With the advent of new technologies, T cells were activated using beads linked to anti-CD 3 and anti-CD 28 antibodies, and the presence of the typical "signal 2" from CD28 no longer needs to be encoded by the CAR itself. Third generation vectors were found to be no better than second generation vectors in vitro assays by using bead activation and did not provide significant benefits relative to second generation vectors in mouse models of leukemia (Haso W, Lee DW, Shah NN, Stetler-Stevenson M, Yuan CM, Pastan IH, Dimitrov DS, Morgan RA, FitzGerald DJ, Barrett DM, Wayne AS, Mackall CL, Orentas RJ.An-CD 22-chimeraanti recording B cell precorsor acid lymphoblastic leukemia, blood.2013; 121 (7): 1165-74; Konderfer JN et al, blood.2012; 119 (27012): 2709-20). This was confirmed by the clinical success of CD 19-specific CAR for the second generation CD28/CD 3-zeta (Lee DW et al, American Society of health evaluation. New Orleans, LA; 12 months, 7 days to 12 months, 10 days in 2013) and CD137/CD 3-zeta signaling forms (Porter DL et al, N Engl J Med.2011; 365 (8): 725-33). In addition to CD137, other tumor necrosis factor receptor superfamily members (e.g., OX40) are also capable of providing important sustained signals in CAR-transduced T cells (Yvon E et al, Clin Cancer Res.2009; 15 (18): 5852-60). Also important are culture conditions under which the CAR T cell population is cultured.
Current challenges in broader and effective adaptation of CAR therapies for cancer are associated with the lack of powerful targets. Establishing conjugates of cell surface antigens is readily achievable today, but finding cell surface antigens that are specific for tumors while sparing normal tissues remains a formidable challenge. One potential way to confer greater target cell specificity to CAR-expressing T cells is to use a combinatorial CAR approach. In one system, the CD 3-zeta and CD28 signaling units are isolated in two different CAR constructs expressed within the same cell; in another system, two CARs are expressed in the same T cell, but one has lower affinity and therefore requires the other CAR to be spliced first (engage) to make the second fully active (Lanitis E et al, Cancer Immunol res.2013; 1 (1): 43-53; Kloss CC et al, Nat biotechnol.2013; 31 (1): 71-5). A second challenge in generating single ScFv-based CARs as immunotherapeutics is tumor cell heterogeneity. At least one team has developed a CAR strategy for glioblastoma in which a population of effector cells simultaneously targets multiple antigens (HER2, IL-13Ra, EphA2), with the desire to avoid the consequences of a negative population of target antigens (Hegde M et al, Mol ther.2013; 21 (11): 2087-.
T cell-based immunotherapy has become a new frontier in synthetic biology; a variety of promoters and gene products are envisioned to direct these highly potent cells to the tumor microenvironment where T cells can not only escape negative regulatory signals but also mediate effective tumor killing. Elimination of unwanted T cells by drug-induced dimerization of the inducible caspase 9 construct with AP1903 suggests a way in which a powerful switch that can control T cell populations can be pharmacologically turned on (Di Stasi a et al, N Engl J med.2011; 365 (18): 1673-83). The generation of effector T cell populations that are immune to the negative regulatory effects of transforming growth factor beta by the expression of decoy receptors further suggests the extent to which effector T cells can be engineered for optimal antitumor activity (Foster AE et al, J Immunother.2008; 31 (5): 500-5). Thus, while it appears that CARs can trigger T cell activation in a manner similar to endogenous T cell receptors, the major hurdles to clinical application of this technology have so far been limited by the in vivo expansion of CAR + T cells, rapid disappearance of cells after infusion, and disappointing clinical activity. A variety of antibody-based modalities are currently being developed to target CD 33-positive tumors, including anti-CD 33 antibody-drug conjugates (Stein A.S. et al, Blood, 2015, 126(23), 324), bispecific T-cell adaptors (BiTEs) (Laszlo GS et al, Blood 2013: 123 (4): 554-. Recent work in preclinical models of AMLIt was shown that lysis of CD33 positive AML blast and tumor cell lines can be achieved in a CD33 targeting mode in vitro and in vivo, but many challenges of this approach become apparent in the Clinical setting, including treatment-related toxicity (available in: world Wide Web businessere. com/news/home/20161227005087/en/Seattle-Genetics-Announc-Clinical-Hold-Phase-1; Rowe JM and Rowe JM)B, Blood 2013121: 4838-4841, Wang QS et al, Mol ther.2015 Jan; 23(1): 184-91, NCT01864902) and suboptimal efficacy (Walter RB et al, blood.2012; 119(26): 6198-6208; cowan AJ et al, Biosci 2013; 18(4): 1311-1334). Furthermore, in BiTE-based approaches, reliance on high-density CD33 antigen expression and the need for additional T-cell costimulation/checkpoint blockade to achieve optimal BiTE function remain challenges (Laszlo GS et al, blood.2014; 123 (4): 554-56, Laszlo GS et al, Blood Cancer Journal (2015)5, e 340). Therefore, there is an urgent and long-standing need in the art for new compositions and methods for treating AML using methods that can exhibit specific and effective anti-tumor effects without the above-mentioned disadvantages.
The present invention addresses these needs by providing CAR compositions and therapeutic methods that can be used to treat cancer and other diseases and/or disorders. In particular, the invention as disclosed and described herein provides CARs useful for treating diseases, disorders, or conditions associated with dysregulated CD33 expression, and which comprise a CD33 antigen binding domain that exhibits high surface expression on transduced T cells, exhibits high cell lysis and in vivo expansion and persistence of transduced T cells.
Disclosure of Invention
Provided herein are novel anti-CD 33 antibodies or antigen-binding domains thereof and Chimeric Antigen Receptors (CARs) comprising such CD33 antigen-binding domains, as well as host cells (e.g., T cells) expressing the receptors, and nucleic acid molecules encoding the receptors. The CAR may consist of a single molecule expressed on the surface of an effector cell, or the CAR comprises a signal transduction module expressed by an effector cell and a soluble targeting module, e.g., when the soluble targeting module binds to the signal transduction module expressed by a cell, a fully functional CAR is formed. CARs exhibit high surface expression on transduced T cells, with a high degree of cell lysis and in vivo expansion and persistence of the transduced T cells. Also provided are methods of using the disclosed CARs, host cells, and nucleic acid molecules, e.g., to treat cancer in a subject.
Accordingly, in one aspect, there is provided an isolated polynucleotide encoding a human anti-CD 33 antibody or fragment thereof, comprising a sequence selected from the group consisting of SEQ ID NOs: 1. 3, 5,7, 9 and 11.
In one embodiment, an isolated polynucleotide is provided encoding a fully human anti-CD 33 antibody or fragment thereof, wherein the antibody or fragment thereof comprises a sequence selected from the group consisting of Fab fragments, F (ab')2Fragments, Fv fragments and fragments of single-chain Fv (ScFv).
In one embodiment, an isolated polynucleotide is provided encoding a fully human anti-CD 33 antibody or fragment thereof, wherein the antibody or fragment thereof comprises a sequence selected from the group consisting of SEQ ID NOs: 2. 4,6, 8, 10 and 12.
In one aspect, an isolated nucleic acid molecule encoding a Chimeric Antigen Receptor (CAR) comprising, from N-terminus to C-terminus, at least one CD33 antigen binding domain, at least one transmembrane domain, and at least one intracellular signaling domain, the CD33 antigen binding domain consisting of a polypeptide comprising an amino acid sequence selected from the group consisting of SEQ ID NOs: 1. 3, 5,7, 9 and 11, or a pharmaceutically acceptable salt thereof.
In one embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded extracellular CD33 antigen-binding domain comprises at least one single-chain variable fragment of an antibody that binds to CD 33.
In another embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded extracellular CD33 antigen-binding domain comprises at least one heavy chain variable region of an antibody that binds to CD 33.
In one embodiment, the targeting domain of the CAR is independently expressed in the form of a monoclonal antibody, ScFv Fab, Fab' 2 and comprises an antigen targeting domain comprising a sequence selected from the group consisting of SEQ ID NO: 1. 3, 5,7, 9 and 11, and the effector cell expression component of the CAR comprises a binding domain specific for binding to a tag or epitope expressed on the soluble CAR moiety, e.g., specific binding of the soluble component of the CAR to the cell binding component of the CAR forms a fully functional CAR structure.
In one embodiment, the targeting domain of the CAR is independently expressed in the form of a monoclonal antibody, ScFv Fab, Fab' 2 and comprises an antigen targeting domain comprising an amino acid sequence selected from the group consisting of SEQ ID NO: 1. 3, 5,7, 9 and 11, and the effector cell expression component of the CAR comprises a tag or epitope that specifically reacts with an additional scFv expressed on the soluble CAR moiety, e.g., specific binding of the soluble component of the CAR to the cell binding component of the CAR forms a fully functional CAR structure.
In another embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded CAR extracellular CD33 antigen binding domain further comprises at least one lipocalin-based antigen binding antigen (anticalin) that binds to CD 33.
In one embodiment, an isolated nucleic acid molecule is provided wherein the encoded extracellular CD33 antigen binding domain is linked to a transmembrane domain by a linker domain.
In another embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded CD33 extracellular antigen-binding domain is preceded by a sequence encoding a leader peptide or a signal peptide.
In another embodiment, an isolated nucleic acid molecule is provided that encodes a CAR comprising at least one CD33 antigen binding domain encoded by a polypeptide comprising an amino acid sequence selected from the group consisting of SEQ ID NOs: 1. 3, 5,7, 9, and 11, and wherein the CAR further encodes an extracellular antigen-binding domain that targets an antigen including, but not limited to, CD19, CD20, CD22, ROR1, mesothelin (mesothelin), CD33, CD38, CD123(IL3RA), CD138, BCMA (CD269), GPC2, GPC3, 4, c-Met, PSMA, glycolipid F77, EGFRvIII, GD-2, NY-ESO-1TCR, MAGE a3 TCR, or any combination thereof.
In certain embodiments, isolated nucleic acid molecules are provided that encode a CAR, wherein the additional encoded extracellular antigen-binding domain comprises an anti-CD 19 ScFv antigen-binding domain, an anti-CD 20 ScFv antigen-binding domain, an anti-CD22 ScFv antigen-binding domain, an anti-ROR 1 ScFv antigen-binding domain, an anti-mesothelin ScFv antigen-binding domain, an anti-CD 33 ScFv antigen-binding domain, an anti-CD 38 ScFv antigen-binding domain, an anti-CD 123(IL3RA) ScFv antigen-binding domain, an anti-CD 138 ScFv antigen-binding domain, an anti-BCMA (CD269) ScFv antigen-binding domain, an anti-GPC 2 ScFv antigen-binding domain, an anti-GPC 3 ScFv antigen-binding domain, an anti-FGFR 4 ScFv antigen-binding domain, an anti-c-ScFv antigen-binding domain, an anti-PMSA ScFv antigen-binding domain, a glycolipid F77 ScFv antigen-binding domain, an anti-EGFRvIII antigen-binding domain, An anti-GD-2 ScFv antigen-binding domain, an anti-NY-ESo-1 TCR ScFv antigen-binding domain, an anti-MAGE A3 TCR ScFv antigen-binding domain, or an amino acid sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto, or any combination thereof.
In one aspect, the CARs provided herein further comprise a linker or spacer domain.
In one embodiment, an isolated nucleic acid molecule is provided that encodes a CAR, wherein the extracellular CD33 antigen binding domain, the intracellular signaling domain, or both are linked to the transmembrane domain by a linker or spacer domain.
In one embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded linker domain is derived from the extracellular domain of CD8 or CD28 and is linked to a transmembrane domain.
In another embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded CAR further comprises a transmembrane domain comprising a transmembrane domain of a protein selected from the group consisting of: an α, β, or zeta chain of a T cell receptor, CD28, CD3 epsilon, CD45, CD4, CD5, CD8, CD9, CD16, CD22, CD33, CD37, CD64, CD80, CD86, CD134, CD137, and CD154, or a combination thereof.
In another embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded intracellular signaling domain further comprises a CD3 ζ intracellular domain.
In one embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded intracellular signaling domain is disposed on the C-terminal side relative to the CD3 ζ intracellular domain.
In another embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded at least one intracellular signaling domain comprises a costimulatory domain, a primary signaling domain, or a combination thereof.
In other embodiments, isolated nucleic acid molecules encoding a CAR are provided, wherein the encoded at least one co-stimulatory domain comprises a functional signaling domain of OX40, CD70, CD27, CD28, CD5, ICAM-1, LFA-1(CD11a/CD18), ICOS (CD278), DAP10, DAP12, and 4-1BB (CD137), or a combination thereof.
In one embodiment, an isolated nucleic acid molecule encoding a CAR is provided, further comprising a leader sequence or a signal peptide, wherein the leader or signal peptide nucleotide sequence comprises SEQ ID NO: 13. SEQ ID NO: 39. SEQ ID NO: 41 or SEQ ID NO: 43.
In another embodiment, an isolated nucleic acid molecule encoding a CAR is provided, wherein the encoded leader sequence comprises SEQ ID NO: 14. SEQ ID NO: 40. SEQ ID NO: 42 or SEQ ID NO: 44, or a pharmaceutically acceptable salt thereof.
In one aspect, provided herein is a Chimeric Antigen Receptor (CAR) comprising, from N-terminus to C-terminus, at least one CD33 antigen binding domain, at least one transmembrane domain, and at least one intracellular signaling domain.
In one embodiment, a CAR is provided, wherein the extracellular CD33 antigen-binding domain comprises at least one single chain variable fragment of an antibody that binds an antigen, or at least one heavy chain variable region of an antibody that binds an antigen, or a combination thereof.
In another embodiment, a CAR is provided, wherein the at least one transmembrane domain comprises a transmembrane domain of a protein selected from the group consisting of: an α, β, or zeta chain of a T cell receptor, CD28, CD3 epsilon, CD45, CD4, CD5, CD8, CD9, CD16, CD22, CD33, CD37, CD64, CD80, CD86, CD134, CD137, and CD154, or a combination thereof.
In some embodiments, a CAR is provided, wherein the CAR further encodes an extracellular antigen-binding domain comprising CD19, CD20, CD22, ROR1, mesothelin, CD33, CD38, CD123(IL3RA), CD138, BCMA (CD269), GPC2, GPC3, FGFR4, c-Met, PSMA, glycolipid F77, EGFRvIII, GD-2, NY-ESO-1TCR, MAGE a3 TCR, or an amino acid sequence 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto, or any combination thereof.
In one embodiment, a CAR is provided, wherein the extracellular antigen-binding domain comprises an anti-CD 19 ScFv antigen-binding domain, an anti-CD 20 ScFv antigen-binding domain, an anti-CD22 ScFv antigen-binding domain, an anti-ROR 1 ScFv antigen-binding domain, an anti-mesothelin ScFv antigen-binding domain, an anti-CD 33 ScFv antigen-binding domain, an anti-CD 38 ScFv antigen-binding domain, an anti-CD 123(IL3RA) ScFv antigen-binding domain, an anti-CD 138 ScFv antigen-binding domain, an anti-BCMA (CD269) ScFv antigen-binding domain, an anti-GPC 2 ScFv antigen-binding domain, an anti-GPC 3 ScFv antigen-binding domain, an anti-FGFR 4 ScFv antigen-binding domain, an anti-c-Met ScFv antigen-binding domain, an anti-PMSA antigen-binding domain, an anti-glycolipid F77 ScFv antigen-binding domain, an anti-EGFRvIII antigen-binding domain, an anti-ScFv antigen-binding domain, an anti-GD 2 ScFv antigen-binding domain, An anti-NY-ESo-1 TCR ScFv antigen-binding domain, an anti-MAGE A3 TCR ScFv antigen-binding domain, or an amino acid sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto, or any combination thereof.
In another embodiment, CARs are provided wherein the extracellular antigen-binding domain comprises only an immunoglobulin variable heavy chain (VH) anti-CD 19 antigen-binding domain, an anti-CD 20 VH antigen-binding domain, an anti-CD22 VH antigen-binding domain, an anti-ROR 1 VH antigen-binding domain, an anti-mesothelin VH antigen-binding domain, an anti-CD 33 VH antigen-binding domain, an anti-CD 38 VH antigen-binding domain, an anti-CD 123(IL3RA) VH antigen-binding domain, an anti-CD 138 VH antigen-binding domain, an anti-BCMA (CD269) VH antigen-binding domain, an anti-GPC 2 VH antigen-binding domain, an anti-GPC 3 VH antigen-binding domain, an anti-FGFR 4VH antigen-binding domain, an anti-c-VH antigen-binding domain, an anti-PMSA VH antigen-binding domain, an anti-GPC 77 VH antigen-binding domain, an anti-EGFRvIII antigen-binding domain, an anti-FGFR 4VH antigen-binding domain, an anti-VH antigen-GD-2 VH antigen-binding domain, An anti-NY-ESO-1 TCR VH antigen binding domain, an anti-MAGE a3 TCR VH antigen binding domain, or an amino acid sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto, or any combination thereof.
In another embodiment, a CAR is provided, wherein the extracellular antigen-binding domain comprises a protein or peptide (P) sequence capable of specifically binding a target antigen, which may be derived from a natural or synthetic sequence comprising: an anti-CD 19P antigen-binding domain, an anti-CD 20P antigen-binding domain, an anti-CD 22P antigen-binding domain, an anti-ROR 1P antigen-binding domain, an anti-mesothelin P antigen-binding domain, an anti-CD 33P antigen-binding domain, an anti-CD 38P antigen-binding domain, an anti-CD 123(IL3RA) P antigen-binding domain, an anti-CD 138P antigen-binding domain, an anti-BCMA (CD269) P antigen-binding domain, an anti-GPC 2P antigen-binding domain, an anti-GPC 3P antigen-binding domain, an anti-FGFR 4P antigen-binding domain, an anti-c-Met P antigen-binding domain, an anti-PMSA P antigen-binding domain, an anti-F77P antigen-binding domain, an anti-EGFRvIII P antigen-binding domain, an anti-GD-2P antigen-binding domain, an anti-NY-ESO-1 TCR P antigen-binding domain, an anti-MAGE A3P antigen-binding domain, or an amino acid sequence having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto, or any combination thereof. In another embodiment, a CAR is provided, wherein the at least one intracellular signaling domain comprises a costimulatory domain and a primary signaling domain.
In another embodiment, there is provided a CAR, wherein the at least one intracellular signaling domain comprises a costimulatory domain comprising a functional signaling domain of a protein selected from the group consisting of: OX40, CD70, CD27, CD28, CD5, ICAM-1, LFA-1(CD11a/CD18), ICOS (CD278), DAP10, DAP12, and 4-1BB (CD137), or a combination thereof.
In one embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 15 (LTG 1905 EF1a VH-2 CD33-CD8 TM-41BB-CD3 ζ nucleic acid sequence (FIG. 2A)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 16 (LTG 1905 EF1a VH-2 CD33-CD8 TM-41BB-CD3 ζ amino acid sequence (FIG. 2A)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 17 (LTG 1906 EF1a-VH-4CD33-CD8 TM-41BB-CD3 ζ nucleic acid sequence (FIG. 2B)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 18 (LTG 1906 EF1a-VH-4CD33-CD8 TM-41BB-CD3 ζ amino acid sequence (fig. 2B)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 19 (LTG1936 EF1a ScFv9 CD33 CD8 TM-41BB-CD3 zeta CAR nucleotide sequence (FIG. 2C)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 20 (LTG1936 EF1a ScFv9 CD33 CD8 TM-41BB-CD3 ζ CAR amino acid sequence (fig. 2C)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 21 (LTG1937 EF1a ScFv10 CD33 CD8 TM-41BB-CD3 zeta nucleic acid sequence (FIG. 2D)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 22 (LTG1937 EF1a ScFv10 CD33 CD8 TM-41BB-CD3 amino acid sequence (FIG. 2D)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 23 (LTG1938 EF1a ScFv12 CD33 CD8 TM-41BB-CD3 zeta nucleic acid sequence (FIG. 2E)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 24 (LTG1938 EF1a ScFv12 CD33 CD8 TM-41BB-CD3 ζ amino acid sequence (FIG. 2E)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 25 (LTG1939 EF1a _ ScFv15 CD33 CD8 TM-41BB-CD3 ζ nucleic acid sequence (FIG. 2F)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 26 (LTG1939 EF1a ScFv15 CD33 CD8 TM-41BB-CD3 ζ amino acid sequence (FIG. 2F)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 69 (LTG1927 EF1a-CD33_ 4CD 8 TM-CD28-CD3 zeta nucleic acid sequence (FIG. 12A)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 70 (LTG1927 EF1a-CD33 — 4CD 8 TM-CD28-CD3 ζ amino acid sequence (fig. 12A)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 71 (LTG _ D0033 Ef1a-CD33 _4VH TNFRSF 19H _ TM _ CD28z nucleic acid sequence (FIG. 12B)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 72 (LTG _ D0033(Ef1a-CD33 _4VH TNFRSF 19H _ TM _ CD28z) amino acid sequence (FIG. 12B)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 73 (LTG _ D0034 Ef1a-CD33 _4VH TNFRSF 19H _ TM _4-1BBz nucleic acid sequence (FIG. 12C)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 74 (LTG _ D0034 Ef1a-CD33 _4VH TNFRSF 19H _ TM _4-1BBz amino acid sequence (FIG. 12C)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 87 (LTG _ D0035 Ef1a _ CD33_4VH H CH2 CH3 IgG4_ CD8TM _ CD28z nucleic acid sequence (FIG. 12F)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 88 (LTG _ D0035 Ef1a _ CD33_4VH H CH2 CH3 IgG4_ CD8TM _ CD28z amino acid sequence (fig. 12F)).
In one aspect, the CARs disclosed herein are modified to express or comprise a detectable marker for use in diagnosing, monitoring and/or predicting treatment outcome (e.g., progression-free survival of a cancer patient) or for monitoring the progression of such treatment.
In one embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 75 (LTG _ D0015 Ef1a-CD33 _4VH CD8 BBz T2A tEGFR nucleic acid sequence (FIG. 12D)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 76 (LTG _ D0015 Ef1a-CD33 _4VH CD8 BBz T2A tfegfr amino acid sequence (fig. 12D)).
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 77 (LTG _ D0016 Ef1a-CD33 _4VH CD 828 z T2A tEGFR nucleic acid sequence (FIG. 12E)). In one embodiment, the nucleic acid sequence encodes a polypeptide comprising SEQ ID NO: 78 (LTG _ D0015 Ef1a-CD33 _4VH CD 828 z T2A tfegfr amino acid sequence (fig. 12E)).
In one embodiment, the nucleic acid molecule encoding the disclosed CAR can be contained in a vector, e.g., a viral vector. The vector is a DNA vector, an RNA vector, a plasmid vector, a cosmid vector, a herpes virus vector, a measles virus vector, a lentiviral vector, an adenoviral vector, or a retroviral vector, or a combination thereof.
In certain embodiments, the vector further comprises a promoter, wherein the promoter is an inducible promoter, a tissue-specific promoter, a constitutive promoter, a suicide promoter (suicide promoter), or any combination thereof.
In another embodiment, the CAR-expressing vector may also be modified to include one or more manipulating elements that control CAR T cell expression or eliminate CAR-T cells via a suicide switch. Suicide switches may include, for example, drugs that induce apoptosis-inducing signaling cascades or induce cell death. In a preferred embodiment, the vector expressing the CAR may also be modified to express an enzyme, such as Thymidine Kinase (TK) or Cytosine Deaminase (CD).
In another aspect, host cells comprising a nucleic acid molecule encoding a CAR are also provided. In some embodiments, the host cell is a T cell, e.g., a primary T cell obtained from a subject. In thatIn one embodiment, the host cell is CD8+T cells.
In another aspect, a pharmaceutical composition is provided comprising an anti-tumor effective amount of a population of human T cells, wherein the T cells comprise a nucleic acid sequence encoding a Chimeric Antigen Receptor (CAR), wherein the CAR comprises at least one extracellular antigen-binding domain comprising a CD33 antigen-binding domain comprising the amino acid sequence of SEQ ID No.2, 4,6, 8, 10, or 12, at least one linker domain, at least one transmembrane domain, and at least one intracellular signaling domain, wherein the T cells are T cells of a human having cancer. The cancer includes, inter alia, hematological cancers, such as leukemia (e.g., Chronic Lymphocytic Leukemia (CLL), Acute Lymphocytic Leukemia (ALL), or Chronic Myelogenous Leukemia (CML)), lymphoma (e.g., mantle cell lymphoma, non-Hodgkin's lymphoma, or Hodgkin's lymphoma), or multiple myeloma, or a combination thereof.
In one embodiment, a pharmaceutical composition is provided, wherein the at least one transmembrane domain of the CAR comprises a transmembrane domain of a protein selected from the group consisting of: an α, β, or zeta chain of a T cell receptor, CD28, CD3 epsilon, CD45, CD4, CD5, CD8, CD9, CD16, CD22, mesothelin, CD33, CD37, CD64, CD80, CD86, CD134, CD137, and CD154, or a combination thereof.
In another embodiment, a pharmaceutical composition is provided, wherein the human cancer comprises adult cancer (adult carcinoma) comprising: cancers of the oral and pharyngeal cavity (tongue, mouth, pharynx, head and neck), digestive system (esophagus, stomach, small intestine, colon, rectum, anus, liver, intrahepatic bile duct, gall bladder, pancreas), respiratory system (larynx, lung and bronchi), bone and joint, soft tissue, skin (melanoma, basal cell and squamous cell carcinoma), paediatric tumors (neuroblastoma, rhabdomyosarcoma, osteosarcoma, Ewing's sarcoma), tumors of the central nervous system (brain, astrocytoma, glioblastoma, glioma), and cancers of the breast, reproductive system (cervix, uterus, ovary, vulva, vagina, prostate, testis, penis, endometrium), urinary system (bladder, kidney and renal pelvis, ureter), eye and orbit, endocrine system (thyroid), and brain and other nervous systems, or any combination thereof.
In another embodiment, a pharmaceutical composition is provided comprising an anti-tumor effective amount of a population of human T cells of a human having a cancer, wherein the cancer is a refractory cancer that is not responsive to one or more chemotherapeutic agents. Such cancers include hematopoietic cancers (myelodysplastic cancer), myelodysplastic syndromes, pancreatic cancer, head and neck cancer, skin tumors, Minimal Residual Disease (MRD) among: acute Lymphocytic Leukemia (ALL), Acute Myelogenous Leukemia (AML), adult B-cell malignancies, including CLL (chronic lymphocytic leukemia), CML (chronic myelogenous leukemia), non-hodgkin lymphoma (NHL), pediatric B-cell malignancies, including B lineage ALL (acute lymphocytic leukemia), multiple myeloma, lung cancer, breast cancer, ovarian cancer, prostate cancer, colon cancer, melanoma or other hematological and solid tumors, or any combination thereof.
In another aspect, a method of making a T cell comprising a CAR (hereinafter "CAR-T cell") is provided. The method comprises transducing a T cell with a vector or nucleic acid molecule encoding the disclosed CAR that specifically binds to CD33, thereby producing a CAR-T cell.
In another aspect, there is provided a method of producing an RNA engineered cell population comprising introducing an in vitro transcribed RNA or a synthetic RNA of a nucleic acid molecule encoding a disclosed CAR into a cell of a subject, thereby producing a CAR cell.
In another aspect, there is provided a method for diagnosing a disease, disorder or condition associated with CD33 expression on a cell, comprising: a) contacting the cell with a human anti-CD 33 antibody or fragment thereof, wherein the antibody or fragment thereof comprises an amino acid sequence selected from the group consisting of SEQ ID NOs: 2. 4,6, 8, 10 and 12; and b) detecting the presence of CD33, wherein the presence of CD33 is diagnostic of a disease, disorder or condition associated with CD33 expression.
In one embodiment, the disease, disorder or condition associated with CD33 expression is a cancer, including hematopoietic cancers, myelodysplastic syndrome, pancreatic cancer, head and neck cancer, skin tumors, Minimal Residual Disease (MRD) among: acute Lymphocytic Leukemia (ALL), Acute Myeloid Leukemia (AML), adult B-cell malignancies, including CLL (chronic lymphocytic leukemia), CML (chronic myeloid leukemia), non-hodgkin's lymphoma (NHL), pediatric B-cell malignancies, including B lineage ALL (acute lymphocytic leukemia), multiple myeloma, lung, breast, ovarian, prostate, colon, melanoma, or other hematological and solid tumors, or any combination thereof.
In another embodiment, a method of diagnosing, prognosing or determining the risk of a CD 33-associated disease in a mammal is provided, comprising detecting the expression of CD33 in a sample derived from said mammal, comprising a) contacting said sample with a human anti-CD 33 antibody or fragment thereof, wherein said antibody or fragment thereof comprises an amino acid sequence selected from the group consisting of SEQ ID NOs: 2. 4,6, 8, 10 and 12; and b) detecting the presence of CD33, wherein the presence of CD33 is diagnostic of a CD 33-associated disease in the mammal.
In another embodiment, there is provided a method of inhibiting CD 33-dependent T cell inhibition comprising contacting a cell with a human anti-CD 33 antibody or fragment thereof, wherein the antibody or fragment thereof comprises a heavy chain variable region selected from the group consisting of SEQ ID NOs: 2. 4,6, 8, 10 and 12. In one embodiment, the cell is selected from the group consisting of a tumor cell expressing CD33, a tumor-associated macrophage (tumor-associated macrophage), and any combination thereof.
In another embodiment, a method of blocking T cell inhibition mediated by a cell expressing CD33 and altering the tumor microenvironment to inhibit tumor growth in a mammal is provided comprising administering to the mammal an effective amount of a composition comprising an isolated anti-CD 33 antibody or fragment thereof, wherein the antibody or fragment thereof comprises an amino acid sequence selected from the group consisting of SEQ ID NOs: 2. 4,6, 8, 10 and 12. In one embodiment, the cell is selected from the group consisting of a tumor cell expressing CD33, a tumor-associated macrophage, and any combination thereof.
In another embodiment, a method of inhibiting, suppressing or preventing immunosuppression of an anti-tumor or anti-cancer immune response in a mammal is provided, comprising administering to the mammal an effective amount of a composition comprising an isolated anti-CD 33 antibody or fragment thereof, wherein the antibody or fragment thereof comprises an amino acid sequence selected from the group consisting of SEQ ID NOs: 2. 4,6, 8, 10 and 12. In one embodiment, the antibody or fragment thereof inhibits the interaction between a first cell and a T cell, wherein the first cell is selected from the group consisting of a tumor cell expressing CD33, a tumor-associated macrophage, and any combination thereof.
In another aspect, there is provided a method for inducing anti-tumor immunity in a mammal comprising administering to the mammal a therapeutically effective amount of a T cell transduced with a vector or nucleic acid molecule encoding a disclosed CAR.
In another embodiment, a method of treating or preventing cancer in a mammal is provided comprising administering to the mammal one or more disclosed CARs in an amount effective to treat or prevent cancer in the mammal. The method comprises administering to a subject a therapeutically effective amount of a host cell expressing a disclosed CAR that specifically binds to CD33 and/or one or more of the foregoing antigens under conditions sufficient to form an immune complex on the CAR with the extracellular domain of CD33 and/or one or more of the foregoing antigens in the subject.
In another embodiment, a method is provided for treating a mammal having a disease, disorder or condition associated with elevated expression of a tumor antigen, the method comprising administering to the subject a pharmaceutical composition comprising an anti-tumor effective amount of a population of T cells, wherein the T cells comprise a nucleic acid sequence encoding a Chimeric Antigen Receptor (CAR), wherein the CAR comprises at least one extracellular CD33 antigen binding domain, at least one linker or spacer domain, at least one transmembrane domain, at least one intracellular signaling domain, the extracellular CD33 antigen binding domain comprising the amino acid sequence of SEQ ID No.2, 4,6, 8, 10 or 12, or any combination thereof, and wherein the T cells are T cells of a subject having cancer.
In another embodiment, a method is provided for treating cancer in a subject in need thereof, comprising administering to the subject a pharmaceutical composition comprising an anti-tumor effective amount of a population of T cells, wherein the T cells comprise a nucleic acid sequence encoding a Chimeric Antigen Receptor (CAR), wherein the CAR comprises at least one CD33 antigen binding domain, at least one linker or spacer domain, at least one transmembrane domain, at least one intracellular signaling domain, the CD33 antigen binding domain comprises the amino acid sequence of SEQ ID No.2, 4,6, 8, 10, or 12, or any combination thereof, wherein the T cells are T cells of a subject having cancer. In some embodiments of the foregoing methods, the at least one transmembrane domain comprises an alpha, beta, or zeta chain of a transmembrane T cell receptor, CD28, CD3 epsilon, CD45, CD4, CD5, CD8, CD9, CD16, CD22, mesothelin, CD33, CD37, CD64, CD80, CD86, CD134, CD137, and CD154, or a combination thereof.
In another embodiment, a method for generating a persisting population of genetically engineered T cells in a human diagnosed with cancer is provided. In one embodiment, the method comprises administering to the human a T cell genetically engineered to express a CAR, wherein the CAR comprises at least one CD33 antigen binding domain, at least one transmembrane domain, and at least one intracellular signaling domain, the CD33 antigen binding domain comprises the amino acid sequence of SEQ ID No.2, 4,6, 8, 10, or 12, or any combination thereof, wherein upon administration, the population of persisting genetically engineered T cells or progeny of the T cells persist in the human for at least 1 month, 2 months, 3 months, 4 months, 5 months, 6 months, 7 months, 8 months, 9 months, 10 months, 11 months, 12 months, 2 years, or 3 years.
In one embodiment, the progeny T cells in a human comprise memory T cells. In another embodiment, the T cell is an autologous T cell.
In aspects and embodiments of all methods described herein, any of the aforementioned cancers, diseases, disorders or conditions associated with elevated expression of a tumor antigen can be treated or prevented or ameliorated using one or more CARs disclosed herein.
In another aspect, there is provided a kit (kit) for preparing a chimeric antigen receptor T cell as described above or for preventing, treating or ameliorating any cancer, disease, disorder or condition associated with elevated expression of a tumor antigen in a subject as described above, comprising a container comprising any one of the nucleic acid molecules, vectors, host cells or compositions disclosed above, or any combination thereof, and instructions for using the kit.
It is understood that CARs, host cells, nucleic acids, and methods are also useful beyond the particular aspects and embodiments described in detail herein. The foregoing features and advantages of the present disclosure will become more apparent from the following detailed description, which proceeds with reference to the accompanying figures.
Drawings
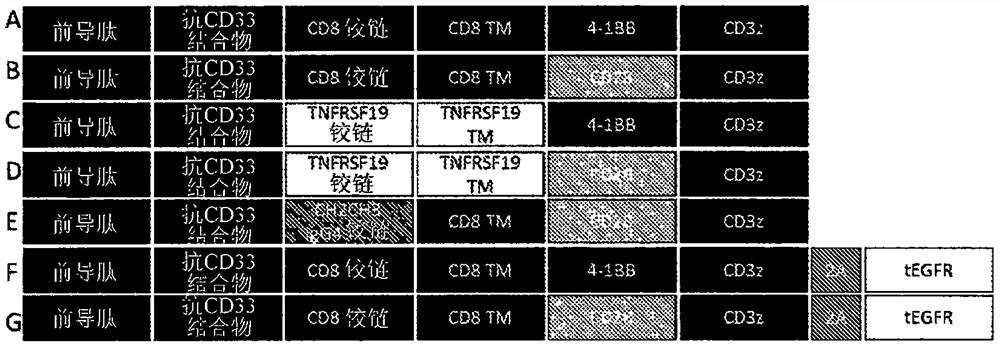
Figure 1 depicts a schematic diagram of the general domain structure of a CAR with a novel extracellular CD33 antigen binding domain sequence. The chimeric antigen receptor comprises an extracellular CD 33-binding immunoglobulin single chain variable fragment (ScFv) domain or just an immunoglobulin heavy chain variable fragment (VH) domain, a hinge domain derived from CD8 (A, B, F, G of fig. 1), TNFRSF19 (C, D of fig. 1), IgG 4(E of fig. 1), a transmembrane domain derived from CD8 (A, B, E, F, G of fig. 1), TNFRSF19 (C, D of fig. 1), an intracellular signal transduction costimulatory domain derived from CD137/4-1BB (A, C, F of fig. 1) or CD28 (B, D, E, G of fig. 1), and a CD3 zeta signal transduction domain. Some bicistronic constructs incorporate a tag derived from truncated egfr (tfegfr) by ribosome skipping 2A sequence (F, G of fig. 1).
Figures 2A-2F depict various Chimeric Antigen Receptors (CARs) comprising novel extracellular CD33 antigen binding domain sequences. The general scheme for CAR includes a signal peptide from N-terminus to C-terminus, an anti-CD 33 conjugate variable heavy chain fragment or a linked single chain variable fragment (ScFv), extracellular linker, transmembrane, 4-1BB, CD3 zeta. FIG. 2A depicts the lentiviral vector expressing the CAR, LTG1905 EF1a VH-2 CD33-CD8 TM-41BB-CD3 zeta nucleic acid sequence and the encoded amino acid sequence. FIG. 2B depicts a lentiviral vector expressing a CAR comprising the LTG1906 (EF1a-VH-4CD33-CD8 TM-41BB-CD3 ζ) nucleic acid sequence and the encoded amino acid sequence. FIG. 2C depicts a lentiviral vector expressing a CAR comprising the LTG1936 EF1a ScFv9 CD33 CD8 TM-41BB-CD3 zeta nucleotide sequence and the encoded amino acid sequence. FIG. 2D depicts a lentiviral vector expressing a CAR comprising the LTG1937 EF1a ScFv10 CD33 CD8 TM-41BB-CD3 zeta nucleic acid sequence and the encoded amino acid sequence. FIG. 2E depicts a lentiviral vector expressing a CAR comprising the LTG1938 EF1a ScFv12 CD33 CD8 TM-41BB-CD3 zeta nucleic acid sequence and the encoded amino acid sequence. FIG. 2F depicts a lentiviral vector expressing a CAR comprising the LTG1939 EF1a ScFv15 CD33 CD8 TM-41BB-CD3 zeta nucleic acid sequence and the encoded amino acid sequence.
Fig. 3 depicts anti-CD 33 CART surface expression in primary human T cells. CAR T cells that were redirected to CD33 tumor antigen via the use of only a variable heavy chain targeting domain were generated by lentiviral transduction. CART detection was performed by flow cytometry. T cells were washed twice in cold PBS-EDTA buffer and stained with CD33-Fc peptide and then with anti-Fc-AF 647 reagent. Data were acquired on a macSQurant 10 flow cytometer in the APC channel. NT untransduced cells, GFP negative control.
Figure 4 depicts anti-CD 33 CAR T cells incorporating immunoglobulin heavy chain variable domain conjugates, demonstrating cell lysis of CD33 positive tumors in vitro. CAR T cells expressing the anti-CD 33 construct were incubated overnight with high CD33(HL-60), medium CD33(K562), and low CD33(Reh) targets stably transduced with firefly luciferase at effector target ratios of 5, 10, and 20. CART cytotoxic activity was then assessed by luciferase activity measurements as described in materials and methods. N3 +/-SEM.
Figure 5 depicts VH-based CD 33-specific CART cells producing high levels of cytokines when co-cultured with a CD33 positive leukemia cell line. anti-CD 33 CART cells were incubated overnight with high CD33(THP-1, HL-60), medium CD33(K562) or low CD33(Reh) leukemia cell lines at an E: T ratio of 10: 1, and supernatants were then analyzed for cytokine concentration by ELISA. N3 +/-SD. Negative control: NT untransduced T cells, 1398-GFP transduced T cells.
Fig. 6 depicts anti-CD 33 CART surface expression in primary human T cells. CAR T cells were generated by lentiviral transduction that were redirected to CD33 tumor antigen via the use of ScFv targeting domains. CAR T detection was performed by flow cytometry. T cells were washed twice in cold PBS-EDTA buffer and stained with CD33-Fc peptide and then with anti-Fc-AF 647 reagent. Data were acquired on a macSQurant 10 flow cytometer in the APC channel. UTD untransduced cells, 1398-GFP negative control.
Figure 7 depicts anti-CD 33 CAR T cells incorporating immunoglobulin heavy chain variable domain conjugates, demonstrating cell lysis of CD33 positive tumors in vitro. CAR T cells expressing the anti-CD 33 construct were incubated overnight with high CD33(HL-60, MOLM-14), medium CD33(K562) and low CD33(Reh) targets stably transduced with firefly luciferase at effector target ratios of 5, 10 and 20. CART cytotoxic activity was then assessed by luciferase activity measurements as described in materials and methods. N3 +/-SEM.
Figure 8 depicts scFv-based and VH-based CD 33-specific CAR T cells producing high levels of cytokines when co-cultured with a CD33 positive leukemia cell line. anti-CD 33 CART cells were incubated overnight with either high CD33(HL-60, MOLM-14) or low CD33(Reh) leukemia cell lines at a 1: 1E: T ratio, and supernatants were then analyzed for cytokine concentration by ELISA. N3 +/-SD. Negative control: UTD-untransduced T cells, 1398-GFP transduced T cells.
Figure 9 depicts CAR T cells expressing multiple anti-CD 33 constructs with HL-60 CD33+Long-term co-incubation assay of tumor cells. Contacting an anti-CD 33 CAR T cell line with HL-60 CD33+Tumor cells were pooled in culture at the indicated effector target (E: T) ratio and maintained for 11 days. The co-cultured cells were then harvested and obtained by flow cytometry. Cells were gated on single and side scatter single peak and dead cells were excluded by 7-AAD staining as described in materials and methods. Boxes indicate the survival HL-60 of each marker under each condition+Tumor cells and CD3+CAR T cellsPercentage of (c). UTD-untransduced T cell control, 1398-GFP transduced T cell control, E: T1: 0 represent T cell only control.
Figure 10 depicts tumor rejection kinetics of CD 33-targeted CAR T cells evaluated in vivo using bioluminescent imaging. NSG mice were inoculated with 1.0x10 on day 06Individual MOLM-14CD33+AML cells and 5.0x10 administered on study day 56A CAR T+Cells/mouse. Tumor burden was assessed weekly by bioluminescence imaging between days 14-35. A. Mean radiation +/-SEM, N6 mice/group. kaplan-Meier curve, depicting the percentage of mice surviving in each experimental group during the course of the experiment, N-6 mice/group. TA-tumor only, UTD-untransduced T cell control.
Figure 11 depicts the function of CD 33-targeted CAR T cells evaluated in vivo. On day 0, NSG mice were inoculated 1.0x106Individual MOLM-14CD33+AML cells and 5.0x10 administered on study day 56A CAR T+Cells/mouse. Blood was collected from mice on study day 19 and analyzed for circulating CAR T, tumor cells, and levels of inflammatory cytokines. A. CART cells and MOLM-14 tumor cells were obtained by flow cytometry, and the absolute cell number was determined using CountBright beads. B. Levels of inflammatory cytokines in mouse plasma were assessed by MACS Human Multiplex Bead Array (MACS Human Multiplex Bead Array). N-6 mice/group. TA-tumor only, UTD-untransduced T cell control. Group comparisons were performed by two-way analysis of variance and Dunnett post test. P < 0.001, p < 0.05, NS-not significant.
Figures 12A-12F depict various Chimeric Antigen Receptors (CARs) comprising novel extracellular VH CD33_4 antigen binding domain sequences, with different CAR configurations. The general scheme for the CAR includes a signal peptide from N-terminus to C-terminus, an anti-CD 33 conjugate variable heavy chain fragment extracellular linker, a transmembrane domain, a costimulatory domain, and a CD3 zeta activation domain. Some sequences include a tfegfr tag peptide downstream of the CAR sequence separated by a 2A ribosome skip sequence. Figure 12A depicts a lentiviral vector expressing a CAR comprising the LTG1927 EF1a CD33_ 4CD 8TM CD28 CD3 ζ nucleic acid sequence and encoded amino acid sequence. Figure 12B depicts a lentiviral vector expressing a CAR comprising LTG _ D0033 EF1a CD33_4VH TNFRSF 19H _ TM _ CD28 ζ nucleic acid sequence and encoded amino acid sequence. Figure 12C depicts a lentiviral vector expressing a CAR comprising LTG _ D0034 Ef1a _ CD33_4VH TNFRSF 19H _ TM _4-1BB CD3 ζ nucleic acid sequence and encoded amino acid sequence. Figure 12D depicts a lentiviral vector expressing a CAR comprising LTG _ D0015 CD33_4VH CD8 BB CD3 ζ T2A tfegfr nucleic acid sequence and encoding amino acid sequence. Figure 12E depicts a lentiviral vector expressing a CAR comprising LTG _ D0016 CD33_4VH CD 828 CD3 ζ T2A tfegfr nucleic acid sequence and encoding amino acid sequence. Figure 12F depicts a lentiviral vector expressing a CAR comprising LTG _ D0035 Ef1a _ CD33_4VH H CH2 CH3 IgG4_ CD8TM _ CD28 CD3 ζ nucleic acid sequence and encoded amino acid sequence.
Detailed Description
Definition of
As used herein, a noun without a quantitative modification means one or more unless the context clearly dictates otherwise. For example, the term "antigen" includes one or more antigens and can be considered equivalent to the phrase "at least one antigen". The term "comprising" as used herein means "including". Thus, "comprising an antigen" means "including an antigen" without excluding other elements. The phrase "and/or" means "and" or ". It is also understood that any and all base sizes or amino acid sizes, as well as all molecular weights or molecular mass values given for a nucleic acid or polypeptide are approximate and provided for descriptive purposes, unless otherwise indicated. Although many methods and materials similar or equivalent to those described herein can be used, specific suitable methods and materials are described below. In case of conflict, the present specification, including definitions of terms, will control. In addition, the materials, methods, and examples are illustrative only and not intended to be limiting. To facilitate a review of the various embodiments, the following terminology is provided:
the term "about" when referring to a measurable value (e.g., an amount, a duration, etc.) is meant to encompass variations from a particular value of 20%, or in some cases 10%, or in some cases 5%, or in some cases 1%, or in some cases 0.1%, as such variations are suitable for carrying out the disclosed methods.
Unless otherwise indicated, technical terms herein are used according to conventional usage. Definitions of terms commonly used in molecular biology can be found in Benjamin Lewis, Genes VII, Oxford University Press, 1999; kendrew et al, (ed), The Encyclopedia of Molecular Biology, published by Blackwell Science ltd, 1994; and Robert a.meyers (ed), Molecular Biology and Biotechnology: a Comprehensive Desk Reference, VCH Publishers, Inc., 1995; and other similar references.
The present disclosure provides CD33 antibodies or fragments thereof and Chimeric Antigen Receptors (CARs) having such CD33 antigen binding domains. The functional activity enhancement of the CAR is directly related to the functional activity enhancement of the CAR expressing T cell. As a result of one or more of these modifications, the CARs exhibit both a high degree of cytokine-induced lysis and cell surface expression on transduced T cells, as well as increased levels of T cell expansion in vivo and persistence of transduced CAR-expressing T cells.
The unique ability to combine functional moieties derived from different protein domains is a key innovative feature of Chimeric Antigen Receptors (CARs). The choice of each of these protein domains is a key design feature, as are the ways of their specific combinations. Each design domain is an essential component that can be used between different CAR platforms to engineer the function of lymphocytes. For example, the extracellular binding domain may be selected such that a CAR that is otherwise ineffective becomes effective.
The constant framework components of the immunoglobulin-derived protein sequence used to establish the extracellular antigen-binding domain of the CAR may be completely neutral or it may self-associate and drive the T cell to a state of metabolic failure, thereby making the therapeutic T cell expressing the CAR far less effective. This occurs independently of the antigen binding function of the CAR domain. In addition, the selection of intracellular signaling domains may also control the activity and persistence of the therapeutic lymphocyte population for immunotherapy. While the ability to bind target antigens and the ability to transmit activation signals to T cells via these extracellular and intracellular domains, respectively, are important aspects of CAR design, it has also become apparent that the choice of the source of the extracellular antigen-binding fragment can have a significant impact on the efficacy of the CAR, thus having a limited effect on the function and clinical utility of the CAR.
Surprisingly and unexpectedly, it has now been found that the functional activity of T cells expressing CARs can also be determined using fully human antigen binding domains in CARs rather than using mouse-derived antigen binding fragments that are prone to induce anti-mouse immune responses and CAR T elimination in the host (see, the UPenn-specific clinical using mouse derived SS1 ScFv sequence, NCT 02159716).
The CARs disclosed herein are expressed at high levels in a cell. The CAR-expressing cells have a high in vivo proliferation rate, produce large amounts of cytokines, and have high cytotoxic activity against cells that have CD33 antigen bound to the CAR on their surface. Using the human extracellular CD33 antigen binding domain results in the production of CARs that function better in vivo, while avoiding the induction of anti-CAR immunity in the host immune response, as well as killing the CAR T cell population. CARs expressing the entire human extracellular CD33 ScFv antigen binding domain showed excellent activity/properties, including: i) prevent poor CAR T persistence and function as seen with mouse-derived binding sequences; ii) effective delivery of a region lacking the CAR (i.e., intrapleural); and iii) the ability to generate CAR T cell design based on binders with both high and low affinity to CD 33. The latter property enables researchers to better modulate the efficacy vs toxicity, and/or tissue specificity, of the CAR T product, since lower affinity binders may have higher specificity for tumors than normal tissues, which may prevent off-target tumor toxicity (on-target off tumor toxicity) and bystander cell killing, due to higher CD33 expression on tumors than normal tissues.
The following is a detailed description of the CARs of the invention, including a description of their extracellular CD33 antigen binding domain, transmembrane domain, and intracellular domain, as well as additional descriptions of CARs, antibodies and antigen binding fragments, conjugates, nucleotides, expressions, vectors, and host cells, methods of treatment, compositions, and kits for using the disclosed CARs.
A. Chimeric Antigen Receptor (CAR)
The CARs disclosed herein comprise at least one CD33 antigen binding domain capable of binding to CD33, at least one transmembrane domain, and at least one intracellular domain.
Chimeric Antigen Receptors (CARs) are artificially constructed hybrid proteins or polypeptides comprising an antigen binding domain, such as a single chain variable fragment (ScFv), of an antibody linked to a T cell signaling domain via a transmembrane domain. Features of the CAR include its ability to redirect T cell specificity and reactivity against a selected target in a non-MHC-restricted manner, and the use of the antigen-binding properties of monoclonal antibodies. non-MHC restricted antigen recognition confers CAR-expressing T cells the ability to recognize antigen independently of antigen processing, thereby bypassing the major mechanism of tumor escape. Furthermore, when expressed in T cells, the CARs advantageously do not dimerize with endogenous T Cell Receptor (TCR) alpha and beta chains.
As disclosed herein, the intracellular T cell signaling domain of the CAR can comprise, for example, a T cell receptor signaling domain, a T cell costimulatory signaling domain, or both. A T cell receptor signaling domain refers to the portion of the CAR that comprises the intracellular domain of the T cell receptor, for example, the intracellular portion of a protein such as, but not limited to, CD3 zeta. A costimulatory signaling domain refers to the portion of the CAR that comprises the intracellular domain of a costimulatory molecule, a cell surface molecule other than the antigen receptor or its ligand that is required for an effective response of lymphocytes to an antigen.
1. Extracellular domains
In one embodiment, the CAR comprises a target-specific binding member, which is also referred to as an antigen-binding domain or portion. The choice of domain depends on the type and number of ligands that define the surface of the target cell. For example, the antigen binding domain can be selected to recognize ligands that serve as cell surface markers on target cells associated with a particular disease state. Thus, some examples of cell surface markers that can serve as ligands for the antigen binding domain in a CAR include those associated with viral, bacterial and parasitic infections, autoimmune diseases, and cancer cells.
In one embodiment, the CAR can be engineered to target a tumor antigen of interest by engineering a desired antigen binding domain that specifically binds to the antigen on the tumor cell. Tumor antigens are proteins produced by tumor cells that elicit an immune response, particularly a T cell-mediated immune response. The choice of antigen binding domain will depend on the particular type of cancer to be treated. Tumor antigens include, for example, glioma-associated antigen, carcinoembryonic antigen (CEA), β -human chorionic gonadotropin, alpha-fetoprotein (AFP), lectin-reactive AFP, thyroglobulin, RAGE-1, MN-CA IX, human telomerase reverse transcriptase, RU1, RU2(AS), enterocarboxyesterase, mut hsp70-2, M-CSF, prostatase, prostate-specific antigen (PSA), PAP, NY-ESO-1, LAGE-1a, p53, prostein, PSMA, Her2/neu, leptin and telomerase, prostate cancer tumor antigen-1 (pro-carcinoma mordant antigen-1, PCTA-1), MAGE, ELF2M, neutrophil elastase, ephrinB2, insulin 22, insulin growth factor (IGF-I, IGF), IGF-growth factor I, IGF, IGF-II, IGF-I receptor and CD 33. The tumor antigens disclosed herein are included by way of example only. This list is not meant to be exclusive and other examples will be apparent to those skilled in the art.
In one embodiment, the tumor antigen comprises one or more antigenic cancer epitopes associated with a malignancy. Malignant tumors express a variety of proteins that can serve as target antigens for immune attack. These molecules include, but are not limited to, tissue-specific antigens such as MART-1, tyrosinase and GP100 in melanoma, and Prostate Acid Phosphatase (PAP) and prostate-specific antigen (PSA) in prostate cancer. Other target molecules belong to the group of transformation-related molecules, for example the oncogene HER-2/Neu/ErbB-2. Another group of target antigens are cancer-embryonic antigens such as carcinoembryonic antigen (CEA). In B-cell lymphomas, tumor-specific idiotype immunoglobulins constitute a true tumor-specific immunoglobulin antigen that is characteristic of an individual's tumor. B cell differentiation antigens (e.g., CD19, CD20, and CD37) are further candidates as target antigens in B cell lymphomas. Some of these antigens (CEA, HER-2, CD19, CD20, idiotype) have been used as targets for passive immunotherapy using monoclonal antibodies, but with limited success.
In a preferred embodiment, the tumor antigen is CD33 and the tumor associated with CD33 expression comprises lung carcinoma mesothelioma, ovarian cancer and pancreatic cancer, or any combination thereof, that expresses high levels of the extracellular protein CD 33.
The type of tumor antigen can also be a tumor-specific antigen (TSA) or a tumor-associated antigen (TAA). TSA is unique to tumor cells and does not appear on other cells in the body. TAAs are not unique to tumor cells and are instead expressed on normal cells under conditions that fail to induce an immune-tolerant state against the antigen. Expression of the antigen on the tumor may occur under conditions that enable the immune system to respond to the antigen. TAA may be an antigen expressed on normal cells during fetal development when the immune system is immature and unable to respond, or it may be an antigen that is normally present at very low levels on normal cells but is expressed at much higher levels on tumor cells.
Non-limiting examples of TSA or TAA include the following: differentiation antigens such as MART-1/Melana (MART-I), gp100(Pmel 17), tyrosinase, TRP-1, TRP-2, and tumor specific multispectral antigens such as MAGE-1, MAGE-3, BAGE, GAGE-1, GAGE-2, p 15; overexpressed embryonic antigens such as CEA; overexpressed oncogenes and mutated tumor suppressor genes, such as p53, Ras, HER-2/neu; unique tumor antigens resulting from chromosomal translocations, such as BCR-ABL, E2A-PRL, H4-RET, IGH-IGK, MYL-RAR; and viral antigens such as EBVA, an Epstein Barr virus (Epstein Barr virus) antigen, and Human Papilloma Virus (HPV) antigens E6 and E7. Other protein-based macroantigens include TSP-180, MAGE-4, MAGE-5, MAGE-6, RAGE, NY-ESO, P185erbB2, P180erbB-3, C-met, nm-23H1, PSA, TAG-72, CA 19-9, CA 72-4, CAM 17.1, NuMa, K-ras, beta-catenin, CDK4, Mum-1, P15, P16, 43-9F, 5T4, 791Tgp72, alpha fetoprotein, beta-HCG, BCA225, BTA, CA 125, CA 15-3\ CA 27.29 BCAA, CA 195, CA 242, CA-50, CAM 5, CD68\ P1, CO-029, G-5, G250, Ga733\ CAM, gp 175-63344, M-6350, MOV-25, SDC 7, SDC-24, GCA-GCGCTC55, GCGCGCGCGCTC9, GCGCTC9, GCTC9, GCTCK-3670, GCATG-24, GCA-3690, GCAS-36387, GCA-binding protein, GCS-24, GCAS-3690, GCA-binding protein, and GCS-6, TAAL6, TAG72, TLP and TPS.
In one embodiment, the antigen binding domain portion of the CAR targets an antigen including, but not limited to: CD19, CD20, CD22, ROR1, CD33, c-Met, PSMA, glycolipid F77, EGFRvIII, GD-2, MY-ESO-1 TCR, MAGE A3 TCR, and the like.
In a preferred embodiment, the antigen binding domain portion of the CAR targets the extracellular CD33 antigen.
In a preferred embodiment, the isolated nucleic acid molecule encoding the extracellular CD33 VH-2 antigen binding domain comprises SEQ ID NO: 1, or a sequence having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto. In one embodiment, an isolated nucleic acid molecule is provided wherein the encoded extracellular CD33 VH-2 antigen binding domain comprises the amino acid sequence of SEQ ID NO: 2, or an amino acid sequence identical to SEQ ID NO: 2, has 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity.
In a preferred embodiment, the isolated nucleic acid molecule encoding the extracellular CD33 VH-4 antigen binding domain comprises SEQ ID NO: 3, or a sequence having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto. In one embodiment, an isolated nucleic acid molecule is provided wherein the encoded extracellular CD33 VH-4 antigen binding domain comprises the amino acid sequence of SEQ ID NO: 4, or an amino acid sequence identical to SEQ ID NO: 4 has an amino acid sequence of 85%, 90%, 95%, 96%, 97%, 98% or 99% identity.
In a preferred embodiment, the isolated nucleic acid molecule encoding an extracellular CD33 ScFv9 antigen binding domain comprises SEQ ID NO: 5, or a sequence having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto. In one embodiment, an isolated nucleic acid molecule is provided, wherein the encoded extracellular CD33 ScFv9 antigen binding domain comprises SEQ ID NO: 6, or an amino acid sequence identical to SEQ ID NO: 6, has 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity.
In a preferred embodiment, the isolated nucleic acid molecule encoding the extracellular CD33 ScFv10 antigen binding domain comprises SEQ ID NO: 7, or a sequence having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto. In one embodiment, an isolated nucleic acid molecule is provided, wherein the encoded extracellular CD33 ScFv10 antigen binding domain comprises the amino acid sequence of SEQ ID NO: 8, or an amino acid sequence identical to SEQ ID NO: 8, has 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity.
In a preferred embodiment, the isolated nucleic acid molecule encoding the extracellular CD33 ScFv12 antigen binding domain comprises SEQ ID NO: 9, or a sequence having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto. In one embodiment, an isolated nucleic acid molecule is provided wherein the encoded extracellular CD33 ScFv12 antigen binding domain comprises SEQ ID NO: 10, or an amino acid sequence identical to SEQ ID NO: 10, having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity.
In a preferred embodiment, the isolated nucleic acid molecule encoding the extracellular CD33 ScFv15 antigen binding domain comprises SEQ ID NO: 11, or a sequence having 85%, 90%, 95%, 96%, 97%, 98%, or 99% identity thereto. In one embodiment, an isolated nucleic acid molecule is provided, wherein the encoded extracellular CD33 ScFv15 antigen binding domain comprises the amino acid sequence of SEQ ID NO: 12, or an amino acid sequence identical to SEQ ID NO: 12 has an amino acid sequence of 85%, 90%, 95%, 96%, 97%, 98% or 99% identity.
The generation and binding characteristics of the specific CD33 described herein are shown in example 1 for only the variable heavy chain and ScFv antigen-binding fragments or antigen binders.
In various embodiments of the CD 33-specific CARs disclosed herein, the general scheme is shown in figure 1 and comprises, from N-terminus to C-terminus, a signal or leader peptide, an anti-CD 33 ScFv, an extracellular linker, CD8 across a membrane, 4-1BB, CD3 ζ, wherein the cloning sites for the linking domains are indicated in bold letters.
In one embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 15 and encodes a nucleic acid sequence comprising SEQ ID NO: 16 [ LTG1905 EF1a VH-2 CD33-CD8 TM-41BB-CD3 ζ amino acid sequence (shown in FIG. 2A) ].
In one embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 15 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto, and encodes a polypeptide comprising the nucleic acid sequence of SEQ ID NO: 16 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto [ LTG1905 EF1a VH-2 CD33-CD8 TM-41BB-CD3 ζ amino acid sequence (as shown in figure 2A) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 17, and encodes a nucleic acid sequence comprising SEQ ID NO: 18 [ LTG1906 EF1a-VH-4CD33-CD8 TM-41BB-CD3 ζ amino acid sequence (shown in FIG. 2B) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 17 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto, and encodes a polypeptide comprising the nucleic acid sequence of SEQ ID NO: 18 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto [ LTG1906 EF1a-VH-4CD33-CD8 TM-41BB-CD3 ζ amino acid sequence (as shown in figure 2B) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 19 and encodes a nucleic acid sequence comprising SEQ ID NO: 20 [ LTG1936 EF1a ScFv9 CD33 CD8 TM-41BB-CD3 ζ CAR amino acid sequence (as shown in figure 2C) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 19 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto and encodes a polypeptide comprising the nucleic acid sequence of SEQ ID NO: 20 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto [ LTG1936 EF1a ScFv9 CD33 CD8 TM-41BB-CD3 ζ CAR amino acid sequence (as shown in figure 2C) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 21 and encodes a nucleic acid sequence comprising SEQ ID NO: 22 [ LTG1937 EF1a ScFv10 CD33 CD8 TM-41BB-CD3 amino acid sequence (as shown in FIG. 2D) ].
In yet another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 21 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto and encodes a polypeptide comprising the nucleic acid sequence of SEQ ID NO: 22 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto [ LTG1937 EF1a ScFv10 CD33 CD8 TM-41BB-CD3 amino acid sequence (as shown in figure 2D) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 23 and encodes a nucleic acid sequence comprising SEQ ID NO: 24 [ LTG1938 EF1a ScFv12 CD33 CD8 TM-41BB-CD3 zeta amino acid sequence (as shown in FIG. 2E) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 23 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto and encodes a polypeptide comprising the nucleic acid sequence of SEQ ID NO: 24 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto [ LTG1938 EF1a ScFv12 CD33 CD8 TM-41BB-CD3 ζ amino acid sequence (as shown in figure 2E) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 25 and encodes a nucleic acid sequence comprising SEQ ID NO: 26 [ (LTG1939 EF1a ScFv15 CD33 CD8 TM-41BB-CD3 ζ amino acid sequence (shown in figure 2F) ].
In another embodiment, the nucleic acid sequence encoding the CAR comprises SEQ ID NO: 25 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto, and encodes a polypeptide comprising the nucleic acid sequence of SEQ ID NO: 26 or a sequence having 85%, 90%, 95%, 96%, 97%, 98% or 99% identity thereto [ (LTG1939 EF1a ScFv15 CD33 CD8 TM-41BB-CD3 ζ amino acid sequence (as shown in figure 2F) ].
Surface expression of anti-CD 33 CARs incorporating immunoglobulin heavy chain variable domain (VH) and single chain variable fragment (ScFv) sequences reactive with CD33 antigen is shown in example 2 below, and summarized in table 2. The expression level of each ScFv or VH containing CAR was determined by flow cytometry analysis of LV transduced T cells from healthy donors using a recombinant CD33-Fc peptide, followed by an anti-human Fc F (ab') 2 fragment conjugated with AF647 and detected in the APC channel (see example 2, figures 3 and 6). VH-based anti-CD 33 CAR constructs 1905 and 1906 (black traces) were readily detected on the surface of T cells from both donors, demonstrating the reproducibility of T cell transduction. In contrast, CAR expression was not detected in negative control non-transduced T cells (grey traces) and GFP control (not shown), thus demonstrating the specificity of the detection method used (see example 2, figure 3 and table 2). Similarly, ScFv-based anti-CD 33 CAR constructs 1936, 1937, 1938, and 1939 were highly expressed in human primary T cells (black traces) compared to untransduced T cell controls (grey traces). Representative results for one donor are shown.
As shown in fig. 4 and 7 of example 2, the high cytolytic activity of CD33 CAR was demonstrated when Lentiviral Vectors (LV) expressing the following CARs were generated and tested for anti-leukemic activity. Each experimental CAR comprised the 4-1BB/CD 3-zeta chain signaling motif and the specific anti-CD 33 binding motif/domain noted herein. Four leukemia target cell lines with different surface expression of CD33 were used: HL-60 and MOLM-14 (high), Reh and K562 (low). VH domain based CAR-T constructs LTG1905 and LTG1906 lysed low CD 33K 562 cells, whereas LTG1906 showed excellent cell lysis function at effector to target (E: T) ratios listed on the x-axis (see figure 4, LTG1905 and LTG1906, black diamonds and circles, respectively). LTG1906, but not LTG1905, showed potent killing function when used in conjunction with high CD33 HL-60 tumor cell lines, highlighting the robustness of construct LTG 1906. In contrast, no specific cytolytic activity was exerted by either negative control group NT (untransduced T cells) and 1398 (T cells transduced via GFP control), so we observed cytolytic activity of anti-CD 33 CAR LTG1906 and LTG1905 on CD33 expressing tumor cell lines, both target-specific and CART-dependent.
In contrast, ScFv-based anti-CD 33 CAR constructs LTG1936 and LTG1939 were able to efficiently lyse the high CD33 tumor cell lines HL-60 and MOLM-14, while they only partially lyse the low CD33 Reh tumor cell line and had no specific lytic activity against K562 (see figure 7, LTG1398 and LTG1936, white squares and white inverted triangles, respectively). This finding demonstrates the efficiency and specificity of the CAR constructs produced. Unexpectedly, the other CAR constructs LTG1937 and LTG1938 tested in this panel were inefficient at lysing high CD33 tumor cell lines, thus again demonstrating that CART design is not trivial and that soluble antibody features cannot be directly translated into CAR function.
anti-CD 33 CAR T cells were then evaluated for their cytokine secretion capacity. Tumor cells were co-incubated with CAR T cells or control T cells at a 10: 1 effector to target ratio overnight and culture supernatants were analyzed for IFN γ, TNF α and IL-2 by ELISA (see figure 5 and table 2). Notably, CAR T expressing cells LTG1905 and LTG1906 produced high levels of IFN γ, TNF α and IL-2, while negative control NT and 1398 groups did not produce appreciable cytokine induction. Unexpectedly, CD33 CAR LTG1905 tended to produce higher levels of induced cytokines against all tumor cell lines tested compared to construct LTG 1906. This result is in contrast to the lower in vitro cell lysis function of LTG1905 compared to LTG1906 (see fig. 4), suggesting that multiple CAR T functional endpoints need to be tested on a construct-by-construct basis.
Without wishing to be limited to any particular mechanism of action, it is believed that possible causes of enhanced therapeutic function associated with the exemplary CARs of the invention include, for example and without limitation: a) lateral movement within the plasma membrane is improved, allowing for more efficient signal transduction; b) superior localization within plasma membrane microdomains (e.g., lipid rafts), and greater ability to interact with transmembrane signaling cascades associated with T cell activation; c) superior localization within the plasma membrane by preferentially moving away from inhibitory or down-regulatory interactions (e.g., less proximity or interaction with phosphatases such as CD 45); and d) excellent assembly into a T cell receptor signaling complex (i.e., an immune synapse); or any combination thereof.
Although the present disclosure has been illustrated with exemplary extracellular CD33 only variable heavy chain and ScFv antigen binding domains, CD33 only other nucleotide and/or amino acid variants within the variable heavy chain and ScFv antigen binding domains can be used to derive the CD33 antigen binding domain for use in the CARs described herein.
Depending on the desired antigen to be targeted, the CAR may additionally be engineered to include a suitable antigen binding domain specific for the desired antigen target. For example, if CD19 is the desired antigen to be targeted, an antibody directed against CD19 can be used as the antigen binding domain incorporated into the CAR.
In an exemplary embodiment, the antigen binding domain portion of the CAR also targets CD 19. Preferably, the antigen binding domain in the CAR is anti-CD 19 ScFV, wherein the nucleic acid sequence of the anti-CD 19 ScFV comprises SEQ ID NO: 37, or a sequence shown in seq id no. In one embodiment, the anti-CD 19 ScFV comprises a nucleic acid sequence encoding SEQ ID NO: 30, or a nucleic acid sequence of the amino acid sequence of 30. In another embodiment, the anti-CD 19 ScFV portion of the CAR comprises SEQ ID NO: 38, or a pharmaceutically acceptable salt thereof.
In one aspect of the invention, there is provided a CAR capable of binding to a non-TSA or non-TAA, including antigens such as but not limited to those derived from: the family of retroviridae (e.g., human immunodeficiency viruses such as HIV-1 and HIV-LP), the family of picornaviridae (e.g., poliovirus, hepatitis a virus, enterovirus, human coxsackievirus, rhinovirus, and echovirus), rubella virus, coronavirus, vesicular stomatitis virus, rabies virus, ebola virus, parainfluenza virus, mumps virus, measles virus, respiratory syncytial virus, influenza virus, hepatitis b virus, parvovirus, adenoviridae, the family of herpesviridae [ e.g., herpes simplex virus types 1 and 2 (HSV), varicella-zoster virus, Cytomegalovirus (CMV), and herpesvirus ], the family of poxviridae (e.g., variola virus, vaccinia virus, and poxvirus virus), or hepatitis c virus, or any combination thereof.
In another aspect of the invention, there is provided a CAR capable of binding to an antigen derived from the following bacterial strain: staphylococcus (Staphyloccci), Streptococcus (Streptococcus), Escherichia coli (Escherichia coli), Pseudomonas (Pseudomonas) or Salmonella (Salmonella). In particular, there is provided a CAR capable of binding to an antigen derived from an infectious bacterium such as: helicobacter pylori (Helicobacter pylori), Legionella pneumophila (Legionella pneumophila), bacterial strains of mycobacterium (mycobacterium sp) (e.g. mycobacterium tuberculosis (m.tuberculosis), mycobacterium avium (m.avium), mycobacterium intracellulare (m.intracellularis), mycobacterium kansasii (m.kansaii) or mycobacterium gordoniae (m.gordonia)), Staphylococcus aureus (Staphylococcus aureus), Neisseria gonorrhoeae (Neisseria gonorrhoeae), Neisseria meningitidis (Neisseria meningitidis), Listeria monocytogenes (Listeria monocytogenes), Streptococcus pyogenes (Streptococcus pneumoniae), Streptococcus Group a (Group a), Streptococcus Group B (Streptococcus B) (Streptococcus pneumoniae), Streptococcus pneumoniae (Clostridium pneumoniae), or Streptococcus pneumoniae (Clostridium Streptococcus pneumoniae), or combinations thereof.
2. Transmembrane domain
With respect to the transmembrane domain, the CAR comprises one or more transmembrane domains fused to the extracellular CD33 antigen binding domain of the CAR.
The transmembrane domain may be derived from natural sources or synthetic sources. If the source is natural, the domain can be derived from any membrane-bound or transmembrane protein.
The transmembrane regions particularly useful in the CARs described herein can be derived from (i.e., comprise at least the following transmembrane regions): the α, β or ζ chain of a T cell receptor, CD28, CD3 ∈, CD45, CD4, CD5, CD8, CD9, CD16, CD22, mesothelin, CD33, CD37, CD64, CD80, CD86, CD134, CD137, CD 154. Alternatively, the transmembrane domain may be synthetic, in which case it will contain predominantly hydrophobic residues such as leucine and valine. Preferably, a triplet of phenylalanine, tryptophan and valine will be present at each end of the synthetic transmembrane domain. Optionally, a short oligopeptide linker or polypeptide linker (preferably 2 to 10 amino acids in length) may form a link between the transmembrane domain and the cytoplasmic signaling domain of the CAR. Glycine-serine diads provide particularly suitable linkers.
In one embodiment, a transmembrane domain that is naturally associated with one of the domains in the CAR is used in addition to the transmembrane domains described above.
In some cases, the transmembrane domains may be selected by amino acid substitutions to avoid binding of such domains to the transmembrane domains of the same or different surface membrane proteins to minimize interaction with other members of the receptor complex.
In one embodiment, the transmembrane domain in the CAR of the invention is the CD8 transmembrane domain. In one embodiment, the CD8 transmembrane domain comprises SEQ ID NO: 27. In one embodiment, the CD8 transmembrane domain comprises a sequence encoding SEQ ID NO: 28, or a nucleic acid sequence of the amino acid sequence of seq id No. 28. In another embodiment, the CD8 transmembrane domain comprises SEQ ID NO: 28.
In one embodiment, the encoded transmembrane domain comprises a polypeptide having the sequence of SEQ ID NO: 28, or an amino acid sequence that is at least one, two, or three modifications (e.g., substitutions) but NO more than 20, 10, or 5 modifications (e.g., substitutions) of the amino acid sequence of SEQ ID NO: 28 has a sequence of 95 to 99% identity.
In some cases, the transmembrane domain of the CAR comprises a CD8a hinge domain. In one embodiment, the CD8 hinge domain comprises SEQ ID NO: 29. In one embodiment, the CD8 hinge domain comprises a nucleotide sequence encoding SEQ ID NO: 30, or a nucleic acid sequence of the amino acid sequence of 30. In another embodiment, the CD8 hinge domain comprises SEQ ID NO: 30, or a sequence having 95 to 99% identity thereto.
In one embodiment, an isolated nucleic acid molecule is provided wherein the encoded linker domain is derived from the extracellular domain of CD8 and is linked to a transmembrane CD8 domain, a transmembrane CD28 domain, or a combination thereof.
In one embodiment, the transmembrane domain in the CAR of the invention is the TNFRSF19 transmembrane domain. In one embodiment, the TNFRSF19 transmembrane domain comprises SEQ ID NO: 51. In one embodiment, TNFRSF19 transmembrane domain comprises a sequence encoding SEQ ID NO: 52. In another embodiment, the TNFRSF19 transmembrane domain comprises SEQ ID NO: 52.
In one embodiment, the encoded transmembrane domain comprises a polypeptide having the sequence of SEQ ID NO: 52, or an amino acid sequence that is at least one, two, or three modifications (e.g., substitutions) but NO more than 20, 10, or 5 modifications (e.g., substitutions) of the amino acid sequence of SEQ ID NO: 52 has a sequence identity of 95 to 99%.
3. Spacer domains
In a CAR, a spacer domain (also referred to as a hinge domain) can be disposed between the extracellular domain and the transmembrane domain, or between the intracellular domain and the transmembrane domain. Spacer domain means any oligopeptide or polypeptide used to link the transmembrane domain to the extracellular domain and/or the transmembrane domain to the intracellular domain. The spacer domain comprises up to 300 amino acids, preferably 10 to 100 amino acids, and most preferably 25 to 50 amino acids.
In some embodiments, the linker may comprise a spacer element, which when present, increases the size of the linker such that the distance between the effector molecule or detectable marker and the antibody or antigen binding fragment is increased. Exemplary spacers are known to those of ordinary skill and include those listed in: U.S. patent nos. 7,964,5667, 498,298, 6,884,869, 6,323,315, 6,239,104, 6,034,065, 5,780,588, 5,665,860, 5,663,149, 5,635,483, 5,599,902, 5,554,725, 5,530,097, 5,521,284, 5,504,191, 5,410,024, 5,138,036, 5,076,973, 4,986,988, 4,978,744, 4,879,278, 4,816,444 and 4,486,414, and U.S. patent publication nos. 20110212088 and 20110070248, each of which is incorporated herein by reference in its entirety.
The spacer domain preferably has a sequence that promotes binding of the CAR to the antigen and enhances signal transduction into the cell. Some examples of amino acids that are expected to facilitate binding include cysteine, charged amino acids, and serine and threonine in potential glycosylation sites, and these amino acids can be used as the amino acids that make up the spacer domain.
As spacer domains, all or part of amino acids 118 to 178 of the hinge region of CD8 alpha (SEQ ID NO: 31) (NCBI RefSeq: NP. sub. - -001759.3), amino acids 135 to 195 of CD8 beta (GenBank: AAA35664.1), amino acids 315 to 396 of CD4 (NCBI RefSeq: NP. sub. - -000607.1) or amino acids 137 to 152 of CD28 (NCBI RefSeq: NP. sub. - -006130.1) can be used. In addition, as the spacer domain, a part of the constant region of the H chain or L chain of an antibody (CH1 region or CL region, for example, a peptide having the amino acid sequence shown in SEQ ID NO: 32) may be used. In addition, the spacer domain may be a synthetic sequence.
In addition, all or part of the amino acids of the constant region of human IgG4(UniProt ID: P01861) comprising CH1 (amino acids 1 to 98), the hinge (SEQ ID NO: 80, and the corresponding nucleotide SEQ ID NO: 79) (amino acids 99 to 110), CH2 (amino acids SEQ ID NO: 81 and the corresponding nucleotide SEQ ID NO: 80) (amino acids 111 to 220), and CH3(SEQ ID NO: 84, and the corresponding nucleotide SEQ ID NO: 83) (amino acids 221 to 327) or combinations thereof may be used, such as the IgG4 hinge CH2 CH3 domain (SEQ ID NO: 86 and the corresponding nucleotide SEQ ID NO: 85).
In one embodiment, the spacer domain of the CAR comprises a TNFRSF19 hinge domain comprising the amino acid sequence of SEQ ID NO: 53. In one embodiment, the TNFRSF19 hinge domain comprises a sequence encoding SEQ ID NO: 54, or a nucleic acid sequence of the amino acid sequence of seq id no. In another embodiment, the TNFRSF19 hinge domain comprises SEQ ID NO: 54 or a sequence having 95 to 99% identity thereto.
In one embodiment, the spacer domain of the CAR comprises a TNFRSF19 truncated hinge domain comprising SEQ ID NO: 55. In one embodiment, the TNFRSF19 truncated hinge domain comprises a sequence encoding SEQ ID NO: 56. In another embodiment, the TNFRSF19 truncated hinge domain comprises SEQ ID NO: 56 or a sequence 95 to 99% identical thereto.
In one embodiment, TNFRSF19 hinge and transmembrane domain comprises SEQ ID NO: 49. In one embodiment, TNFRSF19 hinge and transmembrane domain comprises a sequence encoding SEQ ID NO: 50. In another embodiment, the TNFRSF19 hinge and transmembrane domain comprises SEQ ID NO: 50, or a sequence having 95 to 99% identity thereto.
In one embodiment, the CD8a hinge domain is fused to the TNFRSF19 transmembrane domain comprising SEQ ID NO: 57. In one embodiment, the CD8a hinge domain is fused to the TNFRSF19 transmembrane domain comprising a sequence encoding SEQ ID NO: 58, or a nucleic acid sequence of the amino acid sequence of 58. In another embodiment, the CD8a hinge domain is fused to the TNFRSF19 transmembrane domain comprising SEQ ID NO: 58, or a sequence having 95 to 99% identity thereto.
In addition, in a CAR, a signal peptide sequence (also referred to as a leader peptide) may be attached to the N-terminus. The signal peptide sequence is present at the N-terminus of many secreted and membrane proteins and is 15 to 30 amino acids in length. Since many of the protein molecules mentioned above as intracellular domains have signal peptide sequences, these signal peptides can be used as signal peptides for CARs. In one embodiment, the signal peptide comprises SEQ ID NO: 14, or a pharmaceutically acceptable salt thereof.
In one embodiment, the CD8a leader peptide comprises SEQ ID NO: 43. In one embodiment, the CD8a leader peptide comprises a sequence encoding SEQ ID NO: 44, or a nucleic acid sequence of the amino acid sequence of seq id no. In another embodiment, the CD8a hinge domain has a sequence that is complementary to a sequence comprising SEQ ID NO: 44 or a sequence 95 to 99% identical thereto, and a TNFRSF19 transmembrane domain fused thereto.
In another embodiment, the GMCSF leader peptide comprises SEQ ID NO: 39. In one embodiment, the GMCSF leader peptide comprises a sequence encoding SEQ ID NO: 40. In another embodiment, the CD8a hinge domain has a sequence that is complementary to a sequence comprising SEQ ID NO: 40 or a sequence 95 to 99% identical thereto, to TNFRSF19 transmembrane domain.
In another embodiment, the TNFRSF19 leader peptide comprises SEQ ID NO: 41. In one embodiment, the TNFRSF19 leader peptide and CD8 α leader peptide comprise sequences encoding SEQ ID NOs: 42. In another embodiment, the CD8a hinge domain has a sequence that is complementary to a sequence comprising SEQ ID NO: 42 or a sequence 95 to 99% identical thereto, to TNFRSF19 transmembrane domain.
In one embodiment, the tag sequence encoding a truncated sequence of the epidermal growth factor receptor (tfegfr) comprises SEQ ID NO: 67. In one embodiment, the tfegfr comprises a polypeptide encoding SEQ ID NO: 68. In another embodiment, the tfegfr tag comprises SEQ ID NO: 68, or a sequence having 95 to 99% identity thereto.
In one embodiment, the furin recognition site and downstream T2A self-cleaving peptide sequence designed for simultaneous dicistronic expression of the tag sequence and CAR sequence comprises SEQ ID NO: 65. In one embodiment, the furin and T2A sequences comprise sequences encoding SEQ ID NOs: 66, or a nucleic acid sequence of the amino acid sequence of 66. In another embodiment, the tfegfr tag comprises SEQ ID NO: 66 or a sequence 95 to 99% identical thereto.
In one embodiment, the upstream furin recognition site and the T2A self-cleaving peptide sequence and the furin recognition downstream site designed for simultaneous dicistronic expression of the tag sequence and the CAR sequence comprise SEQ ID NO: 67. In one embodiment, the furin and T2A sequences comprise sequences encoding SEQ ID NOs: 68. In another embodiment, the tfegfr tag comprises SEQ ID NO: 68 or a sequence having 95 to 99% identity thereto.
In one embodiment, the targeting domain of the CAR is expressed separately in the form of a monoclonal antibody, ScFv Fab, Fab' 2 and is comprised in a binding tag or epitope, and the component expressed by the effector cell of the CAR comprises a binding domain specific for binding to a tag or epitope expressed on the soluble CAR moiety, e.g. specific binding of the soluble component of the CAR to the cell binding component forms a fully functional CAR structure.
4. Intracellular domains
The cytoplasmic domain or additional intracellular signaling domain of the CAR is responsible for activating at least one normal effector function of the immune cell in which the CAR has been placed. The term "effector function" refers to a specialized function of a cell. For example, the effector function of a T cell may be cytolytic activity or helper activity, including secretion of cytokines. Thus, the term "intracellular signaling domain" refers to the portion of a protein that transduces effector function signals and directs the cell to perform a specialized function. Although the entire intracellular signaling domain may be used in general, in many cases the entire chain need not be used. To the extent that truncated portions of intracellular signaling domains are used, such truncated portions may be used in place of the entire chain, so long as they transduce effector functional signals. The term intracellular signaling domain is therefore meant to include any truncated portion of an intracellular signaling domain sufficient to transduce an effector function signal.
Some preferred examples of intracellular signaling domains for CARs include T Cell Receptors (TCRs) and cytoplasmic sequences of co-receptors that act synergistically to initiate signal transduction upon antigen receptor engagement, as well as any derivative or variant of these sequences and any synthetic sequences with the same functional capacity.
It is known that the signal generated by the TCR alone is not sufficient to fully activate T cells and that a secondary or co-stimulatory signal is also required. Thus, T cell activation can be thought of as being mediated by two distinct classes of cytoplasmic signaling sequences: those that initiate antigen-dependent primary activation by the TCR (primary cytoplasmic signaling sequences) and those that act in an antigen-independent manner to provide secondary or costimulatory signals (secondary cytoplasmic signaling sequences).
The primary cytoplasmic signaling sequence modulates primary activation of the TCR complex in a stimulatory manner or in an inhibitory manner. The primary cytoplasmic signaling sequence that functions in a stimulatory manner may comprise signaling motifs known as immunoreceptor tyrosine-based activation motifs or ITAMs.
Some examples of primary cytoplasmic signaling sequences comprising ITAMs that are particularly useful for the CARs disclosed herein include those derived from TCR ζ (CD3 ζ), FcR γ, FcR β, CD3 γ, CD3 δ, CD3 ε, CD5, CD22, CD79a, CD79b, and CD66 d. Specific non-limiting examples of ITAMs include peptides having the following sequences: amino acids 51 to 164 of CD3 ζ (NCBI RefSeq: NP. sub. - -932170.1), amino acids 45 to 86 of Fc ε RI γ (NCBI RefSeq: NP. sub. - -004097.1), amino acids 201 to 244 of Fc ε RI β (NCBI RefSeq: NP. sub. - -000130.1), amino acids 139 to 182 of CD3 γ (NCBI RefSeq: NP. sub. - -000064.1), amino acids 128 to 171 of CD3 δ (NCBI RefSeq: NP. sub. - -000723.1), amino acids 153 to 207 of CD3 ε (NCBI RefSeq: NP. sub. - -000724.1), amino acids 402 to 495 of CD5 (NCBI Seq: NP.sub. - -48), amino acids 707 to 847 of CD 0022 (NCBI RefSeq: NP. sub. - -63 001762.2), amino acids a to 495 of CD 0022 (NCBI RefSeq: NP. sub. -. 23) and amino acids 177 to 177 of Fc RI P.23), and variants thereof having the same function as these peptides. The amino acid numbering based on the amino acid sequence information of NCBI RefSeq ID or GenBank described herein is based on the full length of the precursor (including signal peptide sequence, etc.) of each protein. In one embodiment, the cytoplasmic signaling molecule in the CAR comprises a cytoplasmic signaling sequence derived from CD3 ζ.
In a preferred embodiment, the intracellular domain of the CAR can be designed to comprise the CD 3-zeta signaling domain alone or in combination with any other desired cytoplasmic domain that can be used in the CAR context. For example, the intracellular domain of the CAR can comprise a CD3 zeta chain portion and a costimulatory signaling region. A costimulatory signaling region refers to the portion of the CAR that comprises the intracellular domain of the costimulatory molecule. Costimulatory molecules are cell surface molecules other than the antigen receptor or its ligand that are required for an effective response of lymphocytes to an antigen. Some examples of such co-stimulatory molecules include CD27, CD28, 4-1BB (CD137), OX40, CD30, CD40, PD-1, ICOS, lymphocyte function-associated antigen-1 (LFA-1), CD2, CD7, LIGHT, NKG2C, B7-H3, and ligands that specifically bind to CD83, and the like. Specific non-limiting examples of such co-stimulatory molecules include peptides having the following sequences: amino acids 236 to 351 of CD2 (NCBI RefSeq: np.sub. - -001758.2), amino acids 421 to 458 of CD4 (NCBI RefSeq: np.sub. - -000607.1), amino acids 402 to 495 of CD5 (NCBI RefSeq: np.sub. - -055022.2), amino acids 207 to 235 of CD8 α (NCBI RefSeq: np.sub. - -001759.3), amino acids 196 to 210 of CD83 (GenBank: AAA35664.1), amino acids 181 to 220 of CD28 (NCBI RefSeq: np.sub. - -006130.1), amino acids 214 to 255 of CD137(4-1BB, NCBI RefSeq: np.sub. - -001552.2), amino acids 241 to 277 of CD134 (seq: 3, NCBI refsub. - -np. 003318.1) and amino acids 166 to 199 of CD134 (NCBI seq: 84), and their functional variants. Thus, although the disclosure herein is primarily exemplified with 4-1BB as the costimulatory signaling element, other costimulatory elements are also within the scope of the disclosure.
The cytoplasmic signaling sequences within the cytoplasmic signaling portion of the CAR can be linked to each other in random or a specific order. Optionally, short oligopeptide linkers or polypeptide linkers (preferably 2 to 10 amino acids in length) may form the linkage. Glycine-serine diads provide particularly suitable linkers.
In one embodiment, the intracellular domain is designed to comprise the signaling domain of CD 3-zeta and the signaling domain of CD 28. In another embodiment, the intracellular domain is designed to comprise the signaling domain of CD 3-zeta and the signaling domain of 4-1 BB. In another embodiment, the intracellular domain is designed to comprise the signaling domain of CD 3-zeta and the signaling domains of CD28 and 4-1 BB.
In one embodiment, the intracellular domain in the CAR is designed to comprise the signaling domain of 4-1BB and the signaling domain of CD 3-zeta, wherein the signaling domain of 4-1BB comprises the amino acid sequence set forth in SEQ ID NO: 33. SEQ ID NO: 45 or SEQ ID NO: 59, and the signaling domain of CD 3-zeta comprises the nucleic acid sequence set forth in SEQ ID NO: 35. SEQ ID NO: 47 or SEQ ID NO: 61, or a nucleic acid sequence as set forth in seq id no.
In one embodiment, the intracellular domain in the CAR is designed to comprise the signaling domain of 4-1BB and the signaling domain of CD 3-zeta, wherein the signaling domain of 4-1BB comprises a light chain sequence encoding SEQ ID NO: 34. SEQ ID NO: 46 or SEQ ID NO: 60, and the signaling domain of CD3- ζ comprises a nucleic acid sequence encoding the amino acid sequence of SEQ ID NO: 36. or SEQ ID NO: 48. or SEQ ID NO: 62, or a nucleic acid sequence of the amino acid sequence of seq id no.
In one embodiment, the intracellular domain in the CAR is designed to comprise the signaling domain of 4-1BB and the signaling domain of CD 3-zeta, wherein the signaling domain of 4-1BB comprises the amino acid sequence set forth in SEQ ID NO: 34. SEQ ID NO: 46 or SEQ ID NO: 60, and the signaling domain of CD 3-zeta comprises the amino acid sequence set forth in SEQ ID NO: 36. SEQ ID NO: 48 or SEQ ID NO: 62, or a pharmaceutically acceptable salt thereof.
In one embodiment, the intracellular domain in the CAR is designed to comprise the signaling domain of CD28 and the signaling domain of CD 3-zeta, wherein the signaling domain of CD28 comprises the amino acid sequences set forth in SEQ ID NOs: 45 or SEQ ID NO: 59, and the signaling domain of CD 3-zeta comprises the nucleic acid sequence set forth in SEQ ID NO: 35. SEQ ID NO: 47 or SEQ ID NO: 61, or a nucleic acid sequence as set forth in seq id no.
In one embodiment, the intracellular domain in the CAR is designed to comprise the signaling domain of CD28 and the signaling domain of CD 3-zeta, wherein the signaling domain of CD28 comprises a light chain variable region encoding SEQ ID NO: 46 or SEQ ID NO: 60, and the signaling domain of CD3- ζ comprises a nucleic acid sequence encoding the amino acid sequence of SEQ ID NO: 36. or SEQ ID NO: 48. or SEQ ID NO: 62, or a nucleic acid sequence of the amino acid sequence of seq id no.
In one embodiment, the intracellular domain in the CAR is designed to comprise the signaling domain of CD28 and the signaling domain of CD 3-zeta, wherein the signaling domain of CD28 comprises the amino acid sequences set forth in SEQ ID NOs: 46 or SEQ ID NO: 60, and the signaling domain of CD 3-zeta comprises the amino acid sequence set forth in SEQ ID NO: 36. SEQ ID NO: 48 or SEQ ID NO: 62, or a pharmaceutically acceptable salt thereof.
Additional description of CAR
Also specifically included within the scope of the invention are functional portions of the CARs disclosed herein. The term "functional portion" when used with reference to a CAR refers to any portion or fragment of one or more CARs disclosed herein that retains the biological activity of the CAR of which it is a part (the parent CAR). Functional portions encompass, for example, those portions of the CAR that retain the ability to recognize a target cell or detect, treat, or prevent a disease to a similar extent, to the same extent, or to a greater extent, as compared to the parent CAR. With reference to the parent CAR, the functional portion can comprise, for example, about 10%, 25%, 30%, 50%, 68%, 80%, 90%, 95% or more of the parent CAR.
The functional portion may comprise additional amino acids at the amino or carboxy terminus or at both ends of the portion that are not present in the amino acid sequence of the parent CAR. Desirably, the additional amino acids do not interfere with the biological function of the functional moiety, e.g., recognizing target cells, detecting cancer, treating or preventing cancer, and the like. More desirably, the additional amino acids enhance the biological activity as compared to the biological activity of the parent CAR.
Included within the scope of the present disclosure are functional variants of the CARs disclosed herein. The term "functional variant" as used herein refers to a CAR, polypeptide, or protein having significant or significant sequence identity or similarity to a parent CAR, which functional variant retains the biological activity of the CAR of which it is a variant. Functional variants encompass, for example, those variants of the CAR described herein (parent CAR) that retain the ability to recognize the target cell to a similar extent, to the same extent, or to a greater extent, as compared to the parent CAR. With reference to a parent CAR, a functional variant can, for example, have at least about 30%, 50%, 75%, 80%, 90%, 98% or more identity in amino acid sequence to the parent CAR.
A functional variant may, for example, comprise the amino acid sequence of a parent CAR with at least one conservative amino acid substitution. Alternatively or additionally, a functional variant may comprise the amino acid sequence of a parent CAR with at least one non-conservative amino acid substitution. In this case, the non-conservative amino acid substitution preferably does not interfere with or inhibit the biological activity of the functional variant. Non-conservative amino acid substitutions can enhance the biological activity of the functional variant, such that the biological activity of the functional variant is increased as compared to the parent CAR.
The amino acid substitution of the CAR is preferably a conservative amino acid substitution. Conservative amino acid substitutions are known in the art and include amino acid substitutions in which an amino acid having a particular physical and/or chemical property is exchanged for another amino acid having the same or similar chemical or physical property. For example, a conservative amino acid substitution can be an acidic/negatively charged polar amino acid in place of another acidic/negatively charged polar amino acid (e.g., Asp or Glu), an amino acid having a non-polar side chain in place of another amino acid having a non-polar side chain (e.g., Ala, Gly, Val, He, Leu, Met, Phe, Pro, Trp, Cys, Val, etc.), a basic/positively charged polar amino acid in place of another basic/positively charged polar amino acid (e.g., Lys, His, Arg, etc.), an uncharged amino acid having a polar side chain in place of another uncharged amino acid having a polar side chain (e.g., Asn, Gin, Ser, Thr, Tyr, etc.), an amino acid having a beta-branched side chain in place of another amino acid having a beta-branched side chain (e.g., He, Thr, and Val), an amino acid having an aromatic side chain in place of another amino acid having, Phe, Trp, and Tyr), and the like.
The CAR can consist essentially of one or more specific amino acid sequences described herein, such that other components (e.g., other amino acids) do not substantially alter the biological activity of the functional variant.
The CAR (including functional portions and functional variants) can be of any length, i.e., can comprise any number of amino acids, so long as the CAR (or functional portion or functional variant thereof) retains its biological activity, e.g., the ability to specifically bind to an antigen, detect diseased cells in a mammal, or treat or prevent a disease in a mammal, etc. For example, the CAR can be about 50 to about 5000 amino acids long, e.g., 50, 70, 75, 100, 125, 150, 175, 200, 300, 400, 500, 600, 700, 800, 900, 1000 or more amino acids in length.
CARs (including functional portions and functional variants of the invention) may comprise synthetic amino acids substituted for one or more naturally occurring amino acids. Such synthetic amino acids are known in the art and include, for example, aminocyclohexanecarboxylic acid, norleucine, -amino-N-decanoic acid, homoserine, S-acetamidomethyl-cysteine, trans-3-and trans-4-hydroxyproline, 4-aminophenylalanine, 4-nitrophenylalanine, 4-chlorophenylalanine, 4-carboxyphenylalanine, β -phenylserine, β -hydroxyphenylalanine, phenylglycine, a-naphthylalanine, cyclohexylalanine, cyclohexylglycine, indoline-2-carboxylic acid, 1,2, 3, 4-tetrahydroisoquinoline-3-carboxylic acid, aminomalonic acid monoamide, N '-benzyl-N' -methyl-lysine, N-acetyl-3-hydroxy-phenylalanine, 4-chlorophenylalanine, 4-carboxyphenylalanine, β -phenylserine, β -hydroxyphenylserine, N ', N' -dibenzyl-lysine, 6-hydroxylysine, ornithine, -aminocyclopentanecarboxylic acid, a-aminocyclohexanecarboxylic acid, a-aminocycloheptane-carboxylic acid, a- (2-amino-2-norbornane) -carboxylic acid, gamma-diaminobutyric acid, beta-diaminopropionic acid, homophenylalanine and a-tert-butylglycine.
The CAR (including functional moieties and functional variants) may be glycosylated, amidated, carboxylated, phosphorylated, esterified, N-acylated, cyclized (by, for example, disulfide bridges) or converted to an acid addition salt and/or optionally dimerized or multimerized, or conjugated.
The CAR (including functional portions and functional variants thereof) may be obtained by methods known in the art. The CAR may be prepared by any suitable method of preparing a polypeptide or protein. Suitable methods for de novo synthesis of polypeptides and proteins are described, for example, in the following references: chan et al, Fmoc Solid Phase Peptide Synthesis, Oxford University Press, Oxford, United Kingdom, 2000; peptide and Protein Drug Analysis, editions Reid, r., Marcel Dekker, inc., 2000; epitope Mapping, eds. Westwood et al, Oxford University Press, Oxford, United Kingdom, 2001; and us patent 5,449,752. In addition, polypeptides and proteins can be recombinantly produced using nucleic acids described herein using standard recombinant methods. See, e.g., Sambrook et al, Molecular Cloning: a Laboratory Manual, third edition, Cold Spring Harbor Press, Cold Spring Harbor, NY 2001; and Ausubel et al, Current Protocols in Molecular Biology, Greene Publishing Associates and John Wiley & Sons, NY, 1994. Additionally, some CARs (including functional portions and functional variants thereof) can be isolated and/or purified from sources such as plants, bacteria, insects, mammals (e.g., rats, humans, etc.). Methods of isolation and purification are well known in the art. Alternatively, the CARs described herein (including functional portions and functional variants thereof) can be commercially synthesized by a company. In this regard, the CAR can be synthetic, recombinant, isolated, and/or purified.
B. Antibodies and antigen binding fragments
One embodiment also provides a CAR, a T cell expressing a CAR, an antibody, or an antigen binding domain or portion thereof that specifically binds to one or more antigens disclosed herein. As used herein, "CAR-expressing T cell" or "CAR T cell" means a T cell that expresses a CAR and has antigen specificity determined by, for example, the antibody-derived targeting domain of the CAR.
As used herein, "antigen binding domain" may include antibodies and antigen binding fragments thereof. The term "antibody" is used herein in the broadest sense and encompasses a variety of antibody structures, including but not limited to monoclonal antibodies, polyclonal antibodies, multispecific antibodies (e.g., bispecific antibodies), and antigen-binding fragments thereof, so long as they exhibit the desired antigen-binding activity. Non-limiting examples of antibodies include, for example, intact immunoglobulins and variants and fragments thereof known in the art that retain binding affinity for an antigen.
A "monoclonal antibody" is an antibody obtained from a population of substantially homogeneous antibodies, i.e., the individual antibodies comprising the population are identical except for possible naturally occurring mutations that may be present in minor amounts. Monoclonal antibodies are highly specific, being directed against a single epitope. The modifier "monoclonal" indicates the character of the antibody as being obtained from a substantially homogeneous population of antibodies, and is not to be construed as requiring production of the antibody by any particular method. In some examples, a monoclonal antibody is an antibody produced by a monoclonal of B lymphocytes or by cells or progeny thereof into which has been transfected nucleic acids encoding the antibody light and heavy chain variable regions (or antigen-binding fragments thereof) of a single antibody. In some examples, the monoclonal antibody is isolated from the subject. Monoclonal antibodies may have conservative amino acid substitutions that have substantially no effect on antigen binding or other immunoglobulin function. Exemplary methods for producing monoclonal Antibodies are known, see, for example, Harlow & Lane, Antibodies, A Laboratory Manual, second edition, Cold Spring Harbor Publications, New York (2013).
Generally, immunoglobulins have a heavy (H) chain and a light (L) chain interconnected by disulfide bonds. Immunoglobulin genes include the kappa, lambda, alpha, gamma, delta, epsilon and mu constant region genes, as well as myriad immunoglobulin variable domain genes. There are two types of light chains: lambda (. lamda.) and kappa (. kappa.). There are five main heavy chain species (or isotypes) that determine the functional activity of an antibody molecule: IgM, IgD, IgG, IgA, and IgE.
Each of the heavy and light chains comprises a constant region (or constant domain) and a variable region (or variable domain; see, e.g., Kindt et al, Kuby Immunology, 6 th edition, w.h.freeman and co., page 91 (2007)). In some embodiments, the heavy and light chain variable regions combine to specifically bind to an antigen. In other embodiments, only the heavy chain variable region is required. For example, naturally occurring Camelidae antibodies consisting of only heavy chains are functional and stable in the absence of light chains (see, e.g., Hamers-Casterman et al, Nature, 363: 446. Biol. 448, 1993; Sheriff et al, nat. struct. biol. 3: 733. 736, 1996). Reference to "VH" or "VH" refers to the variable region of an antibody heavy chain, including the variable region of an antigen-binding fragment of, for example, Fv, ScFv, dsFv or Fab. Reference to "VL" or "VL" refers to the variable domain of an antibody light chain, including the variable domain of an Fv, ScFv, dsFv, or Fab.
The light and heavy chain variable regions comprise a "framework" region interrupted by three hypervariable regions, also known as "complementarity determining regions" or "CDRs" (see, e.g., Kabat et al, Sequences of Proteins of Immunological Interest, u.s.department of Health and Human Services, 1991). The sequences of the framework regions of different light or heavy chains are relatively conserved within a species. The framework regions of an antibody (i.e., the combined framework regions that make up the light and heavy chains) are used to locate and align the CDRs in three-dimensional space.
The CDRs are primarily responsible for binding to an epitope of the antigen. The amino acid sequence boundaries of a given CDR can be readily determined using any of a number of well-known protocols, including those described by: kabat et Al ("Sequences of Proteins of Immunological Interest," fifth edition. Public Health Service, National Institutes of Health, Bethesda, MD, 1991; "Kabat" numbering scheme), Al-Lazikani et Al ("JMB 273, 927;" Chothia "numbering scheme), and Lefranc et Al (" GT unique number for Immunological binding and T l receptor variable domains and Ig perfect V-like domains, "Dev.com. Immunological, 27: 55-77, 2003;" IMGT "numbering scheme). The CDRs of each chain are typically referred to as CDRs 1, CDRs 2, and CDRs 3 (from N-terminus to C-terminus), and are also typically identified by the chain in which the particular CDR is located. Thus, the VH CDR3 is the CDR3 from the heavy chain variable domain of the antibody from which it was found, while the VL CDR1 is the CDR1 from the light chain variable domain of the antibody from which it was found. Light chain CDRs are sometimes referred to as LCDR1, LCDR2, and LCDR 3. The heavy chain CDRs are sometimes referred to as HCDR1, HCDR2, and HCDR 3.
An "antigen-binding fragment" is a portion of a full-length antibody that retains the ability to specifically recognize a homologous antigen, as well as various combinations of such portions. Non-limiting examples of antigen binding fragments include Fv, Fab '-SH, F (ab') 2; a diabody; a linear antibody; single chain antibody molecules (e.g., ScFv); and multispecific antibodies formed from antibody fragments. Antibody fragments include antigen-binding fragments generated by modification of whole antibodies or those synthesized de novo using recombinant DNA methods (see, e.g., Kontermann and Dubel (ed.), Antibody Engineering, volumes 1 to 2, second edition, Springer Press, 2010).
Single chain antibodies (ScFvs) are genetically engineered molecules comprising VH and VL domains of one or more antibodies linked by a suitable polypeptide linker as a genetically fused single chain molecule (see, e.g., Bird et al, Science, 242: 423426, 1988; Huston et al, Proc. Natl. Acad. Sci., 85: 5879585883, 1988; Ahmad et al, Clin. Dev. Immunol., 2012, doi: 10.1155/2012/980250; Marbry, IDrugs, 13: -. The intramolecular orientation of the VH and VL domains in an ScFv is generally not critical for ScFv. Thus, ScFvs (VH domain-linker domain-VL domain; VL domain-linker domain-VH domain) with two possible arrangements can be used.
In dsFv, the heavy and light chain variable chains have been mutated to introduce disulfide bonds to stabilize the association of the chains. Also included are diabodies, which are bivalent bispecific antibodies in which the VH and VL domains are expressed on a single polypeptide chain, but using a linker that is too short to allow pairing between the two domains on the same chain, thereby forcing the domains to pair with the complementary domains of the other chain and generating two antigen binding sites (see, e.g., Holliger et al, Proc. Natl. Acad. Sci., 90: 64446448, 1993; Poljak et al, Structure, 2: 11211123, 1994).
Antibodies also include genetically engineered forms such as chimeric antibodies (e.g., humanized murine antibodies) and heteroconjugate antibodies (e.g., bispecific antibodies). See also Pierce Catalog and Handbook, 1994-; kuby, j., Immunology, third edition, w.h.freeman & co, New York, 1997.
Non-naturally occurring antibodies can be constructed using solid phase peptide synthesis, can be produced recombinantly, or can be obtained, for example, by screening combinatorial libraries consisting of variable heavy and variable light chains, such as Huse et al, Science 246: 1275-1281(1989), which is incorporated herein by reference. These and other methods of making, for example, chimeric, humanized, CDR grafted, single chain and bifunctional antibodies are well known to those skilled in the art (Winter and Harris, immunological. today 14: 243. sup. 246 (1993); Ward et al, Nature 341: 544. sup. 546 (1989); Harlow and Lane, supra, 1988; Hilyard et al, Protein Engineering: A practical approach (IRL Press 1992); Borrabeck, Antibody Engineering, second edition (Oxford University Press 1995); each of which is incorporated herein by reference).
An "antibody that binds to the same epitope" as a reference antibody refers to an antibody that blocks binding of the reference antibody to its antigen by 50% or more in a competition assay, and vice versa, the reference antibody blocks binding of the antibody to its antigen by 50% or more in a competition assay. Antibody competition assays are known, and exemplary competition assays are provided herein.
A "humanized" antibody or antigen-binding fragment comprises a human framework region and one or more CDRs from a non-human (e.g., mouse, rat, or synthetic) antibody or antigen-binding fragment. A non-human antibody or antigen-binding fragment that provides a CDR is referred to as a "donor", and a human antibody or antigen-binding fragment that provides a framework is referred to as a "recipient". In one embodiment, all CDRs in the humanized immunoglobulin are from a donor immunoglobulin. The constant region need not be present, but if it is present, it can be substantially identical to a human immunoglobulin constant region, e.g., at least about 85% to 90% identical, e.g., about 95% or more. Thus, all parts of the humanized antibody or antigen-binding fragment (except possibly the CDRs) are substantially identical to the corresponding parts of the natural human antibody sequence.
A "chimeric antibody" is an antibody comprising sequences derived from two different antibodies, which are typically of different species. In some examples, a chimeric antibody comprises one or more CDRs and/or framework regions from one human antibody and CDRs and/or framework regions from another human antibody.
A "fully human antibody" or "human antibody" is an antibody that comprises sequences from (or derived from) the human genome, and does not comprise sequences from another species. In some embodiments, the human antibody comprises CDRs, framework regions, and (if present) an Fc region from (or derived from) a human genome. Human antibodies can be identified and isolated using techniques for generating antibodies based on sequences derived from the human genome, e.g., by Phage display or using transgenic animals (see, e.g., Barbas et al, Phage display: A Laboratory Manual, first edition New York: Cold Spring Harbor Laboratory Press, 2004. printing; Lonberg, nat. Biotech., 23: 1117. Snap. 1125, 2005; Lonberg, Curr. Opin. Immunol., 20: 450. J. 459, 2008).
The antibody may have one or more binding sites. If more than one binding site is present, the binding sites may be the same as each other or may be different. For example, a naturally occurring immunoglobulin has two identical binding sites, a single chain antibody or Fab fragment has one binding site, while a bispecific or bifunctional antibody has two different binding sites.
Methods of testing the ability of an antibody to bind to any functional portion of a CAR are known in the art and include any antibody-antigen binding assay, such as, for example, Radioimmunoassay (RIA), ELISA, Western blot, immunoprecipitation, and competitive inhibition assays (see, e.g., Janeway et al, infra, U.S. patent application publication No.2002/0197266 a1 and U.S. patent No.7,338,929).
In addition, the CAR, T cell expressing the CAR, antibody, or antigen-binding portion thereof can be modified to include a detectable label, such as, for example, a radioisotope, a fluorophore (e.g., Fluorescein Isothiocyanate (FITC), Phycoerythrin (PE)), an enzyme (e.g., alkaline phosphatase, horseradish peroxidase), and an elemental particle (e.g., a gold particle).
C. Conjugates
A CAR, a T cell expressing a CAR, or a monoclonal antibody or antigen binding fragment thereof having specificity for one or more antigens disclosed herein can be conjugated to an agent, e.g., an effector molecule or a detectable marker, using any number of methods known to those skilled in the art. Both covalent and non-covalent attachment methods may be used. Conjugates include, but are not limited to, molecules in which an effector molecule or detectable marker is covalently linked to an antibody or antigen-binding fragment that specifically binds to one or more antigens disclosed herein. One skilled in the art will appreciate that a variety of effector molecules and detectable markers may be used, including, but not limited to, chemotherapeutic agents, anti-angiogenic agents, toxins, radioactive agents (e.g., as described above)125I、32P、14C、3H and35s) and other labels, target moieties and ligands, etc.
The choice of a particular effector molecule or detectable marker depends on the particular target molecule or cell, and the desired biological effect. Thus, for example, the effector molecule may be a cytotoxin that is used to cause death of a particular target cell (e.g., a tumor cell).
Manipulation for linking an effector molecule or detectable marker to an antibody or antigen-binding fragment according to effectThe chemical structure of the substance. The polypeptide typically comprises a variety of functional groups, such as carboxylic acid groups (COOH), free amine groups (-NH), which can be used to react with suitable functional groups on the antibody to allow binding of the effector molecule or detectable marker2) Or a mercapto group (-SH). Alternatively, the antibody or antigen-binding fragment is derivatized to expose or attach additional reactive functional groups. Derivatization may involve attaching any of a variety of known linker molecules, such as those available from Pierce Chemical Company, Rockford, IL. The linker may be any molecule used to link the antibody or antigen-binding fragment to an effector molecule or detectable marker. The linker is capable of forming a covalent bond with the antibody or antigen-binding fragment and with the effector molecule or detectable marker. Suitable linkers are well known to those skilled in the art and include, but are not limited to, straight or branched chain carbon linkers, heterocyclic carbon linkers, or peptide linkers. When the antibody or antigen binding fragment and the effector molecule or detectable marker is a polypeptide, the linker may be attached to the constituent amino acids through its side groups (e.g., through disulfide bonds to cysteine) or to the alpha carbon amino and carboxyl groups of the terminal amino acids.
In several embodiments, the linker may comprise a spacer element, which when present, increases the size of the linker such that the distance between the effector molecule or detectable marker and the antibody or antigen binding fragment is increased. Exemplary spacers are known to those of ordinary skill and include those listed in: U.S. patent nos. 7,964,5667, 498,298, 6,884,869, 6,323,315, 6,239,104, 6,034,065, 5,780,588, 5,665,860, 5,663,149, 5,635,483, 5,599,902, 5,554,725, 5,530,097, 5,521,284, 5,504,191, 5,410,024, 5,138,036, 5,076,973, 4,986,988, 4,978,744, 4,879,278, 4,816,444 and 4,486,414, and U.S. patent publication nos. 20110212088 and 20110070248, each of which is incorporated herein by reference in its entirety.
In some embodiments, the linker is cleavable under intracellular conditions such that cleavage of the linker releases the effector molecule or detectable marker from the antibody or antigen binding fragment in an intracellular environment. In other embodiments, the linker is non-cleavable and the effector molecule or detectable marker is released, e.g., by antibody degradation. In some embodiments, the linker can be cleaved by a cleavage agent present in the intracellular environment, e.g., within a lysosome or endosome or pocket (caveolea). The linker may be, for example, a peptide linker that is cleaved by an intracellular peptidase or protease, including but not limited to lysosomal or endosomal proteases. In some embodiments, the peptide linker is at least 2 amino acids long or at least 3 amino acids long. However, the linker may be 4,5, 6,7, 8,9, 10, 11, 12, 13, 14, or 15 amino acids long, e.g., 1 to 2, 1 to 3, 2 to 5,3 to 10, 3 to 15, 1 to 5,1 to 10, 1 to 15 amino acids long. Proteases may include cathepsin B and cathepsin D as well as plasmin, all of which are known to hydrolyze dipeptide drug derivatives such that the active drug is released within the target cell (see, e.g., Dubowchik and Walker, 1999, pharm. For example, a peptide linker (e.g., a phenylalanine-leucine or glycine-phenylalanine-leucine-glycine linker) that can be cleaved by the thiol-dependent protease cathepsin-B can be used. Further examples of such linkers are described, for example, in U.S. Pat. No.6,214,345, which is incorporated herein by reference. In a specific embodiment, the peptide linker that can be cleaved by an intracellular protease is a valine-citrulline linker or a phenylalanine-lysine linker (see, e.g., U.S. Pat. No.6,214,345, which describes the synthesis of doxorubicin using a valine-citrulline linker).
In other embodiments, the cleavable linker is pH sensitive, i.e., sensitive to hydrolysis at a particular pH value. Typically, the pH-sensitive linker is hydrolyzable under acidic conditions. For example, acid-labile linkers that are hydrolyzable in lysosomes (e.g., hydrazones, semicarbazones, thiosemicarbazones, cis-aconitamides, orthoesters, acetals, ketals, etc.) may be used. (see, e.g., U.S. Pat. Nos. 5,122,368; 5,824,805; 5,622,929; Dubowchik and Walker, 1999, pharm. therapeutics 83: 67-123; Neville et al, 1989, biol. chem.264: 14653-14661.) such linkers are relatively stable under neutral pH conditions (e.g., those in blood), but are unstable below pH 5.5 or pH 5.0 (the approximate pH of lysosomes). In certain embodiments, the hydrolyzable linker is a thioether linker (e.g., such as a thioether linked to the therapeutic agent via an acylhydrazone bond) (see, e.g., U.S. patent No.5,622,929).
In other embodiments, the linker is cleavable under reducing conditions (e.g., a disulfide linker). Various disulfide linkers are known in the art, including, for example, those that can be formed using: SATA (N-succinimide-S-acetylthioacetate), SPDP (N-succinimide-3- (2-pyridyldithio) propionate), SPDB (N-succinimide-3- (2-pyridyldithio) butyrate), and SMPT (N-succinimide-oxycarbonyl- α -methyl- α - (2-pyridyldithio) toluene) -, SPDB, and SMPT. (see, e.g., Thorpe et al, 1987, Cancer Res.47: 5924-. See also U.S. patent No.4,880,935).
In other embodiments, the linker is a malonate linker (Johnson et al, 1995, Anticancer Res.15: 1387-93), a maleimidobenzoyl linker (Lau et al, 1995, Bioorg-Med-chem.3 (10): 1299-1304), or a 3' -N-amide analog (Lau et al, 1995, Bioorg-Med-chem.3 (10): 1305-12).
In other embodiments, the linker is non-cleavable and the effector molecule or detectable marker is released by degradation of the antibody. (see U.S. publication No.2005/0238649, which is incorporated herein by reference in its entirety).
In several embodiments, the linker is resistant to cleavage in an extracellular environment. For example, when the conjugate is present in an extracellular environment (e.g., in plasma), no more than about 20%, no more than about 15%, no more than about 10%, no more than about 5%, no more than about 3%, or no more than about 1% of the linker in the conjugate sample is cleaved. Whether a linker is resistant to cleavage in the extracellular environment can be determined, for example, as follows: the conjugate comprising the linker of interest is incubated with plasma for a predetermined time (e.g., 2 hours, 4 hours, 8 hours, 16 hours, or 24 hours) and the amount of free effector molecule or detectable marker present in the plasma is then quantified. Various exemplary linkers that can be used in the conjugates are described in WO 2004-010957, U.S. publication No.2006/0074008, U.S. publication No.20050238649, and U.S. publication No.2006/0024317, each of which is incorporated herein by reference in its entirety.
In several embodiments, conjugates of the CAR, the T cell expressing the CAR, the antibody, or antigen binding portion thereof, and one or more small molecule toxins, such as calicheamicin (calicheamicin), maytansinoids, dolastatins, auristatins, trichothecenes, and CC1065, as well as toxin-active derivatives of these toxins, are provided.
Maytansinoid compounds suitable for use as maytansinoid toxin moieties are well known in the art and may be isolated from natural sources according to known methods, may be produced using genetic engineering techniques (see Yu et al, (2002) PNAS 99: 7968-. Maytansinoids are mitotic inhibitors that act by inhibiting tubulin polymerization. Maytansine was first isolated from the east African shrub Maytenus serrata (Maytenus serrata) (U.S. Pat. No.3,896,111). Subsequently, it was discovered that certain microorganisms also produce maytansinoids, such as maytansinol and C-3 maytansinol esters (U.S. Pat. No.4,151,042). Synthetic maytansinol and derivatives and analogues thereof are disclosed, for example, in the following: U.S. Pat. Nos. 4,137,230; 4,248,870, respectively; 4,256,746, respectively; 4,260,608, respectively; 4,265,814, respectively; 4,294,757, respectively; 4,307,016, respectively; 4,308,268, respectively; 4,308,269, respectively; 4,309,428, respectively; 4,313,946, respectively; 4,315,929, respectively; 4,317,821, respectively; 4,322,348, respectively; 4,331,598, respectively; 4,361,650, respectively; 4,364,866, respectively; 4,424,219, respectively; 4,450,254, respectively; 4,362,663 and 4,371,533, each of which is incorporated herein by reference. Conjugates comprising maytansinoids, methods for their preparation, and their therapeutic use are described, for example, in U.S. Pat. nos. 5,208,020; 5,416,064; 6,441,163 and european patent EP 0425235B 1, the disclosures of which are expressly incorporated herein by reference.
The additional toxin can be used with the CAR, the T cell expressing the CAR, the antibody, or an antigen binding portion thereof. Exemplary toxins include Pseudomonas Exotoxin (PE), ricin, abrin, diphtheria toxin and subunits thereof, ribotoxin (ribotoxin), ribonuclease, saporin, and calicheamicin, and botulinum toxins a through F. These toxins are well known in the art and many are readily available from commercial sources (e.g., Sigma Chemical Company, st. Contemplated toxins also include variants of the toxins (see, e.g., U.S. patent nos. 5,079,163 and 4,689,401).
Saporin is a toxin derived from Saponaria officinalis (Saponaria officinalis) that disrupts protein synthesis by inactivating the 60S portion of the ribosomal complex (Stirpe et al, Bio/Technology, 10: 405, 412, 1992). However, this toxin does not have a mechanism for specific entry into the cell, and therefore needs to be conjugated to an internalized antibody or antigen-binding fragment that recognizes a cell surface protein for efficient uptake by the cell.
Diphtheria toxin was isolated from Corynebacterium diphtheriae (Corynebacterium diphtheriae). Typically, diphtheria toxins used in immunotoxins are mutated to reduce or eliminate non-specific toxicity. A mutant called CRM107 with complete enzymatic activity but significantly reduced non-specific toxicity was known since the 70's of the 20 th century (Laird and Groman, J.Virol.19: 220, 1976) and has been used in human clinical trials. See U.S. Pat. No.5,792,458 and U.S. Pat. No.5,208,021.
Ricin is the lectin RCA60 from Castor (Ricinus communis) (Castor bean). For some examples of ricin, see U.S. patent No.5,079,163 and U.S. patent No.4,689,401. Ricinus Communis Agglutinin (RCA) exists in two forms, which are designated RCA according to their molecular weights of about 65kD and 120kD, respectively60And RCA120(Nicholson &Blaustein, j.biochim.biophysis.acta 266: 543, 1972). The a chain is responsible for inactivating protein synthesis and killing cells. The B chain binds ricin to cell surface galactose residues and facilitates transport of the A chain into the cytosol (Olsnes et al, Nature 249: 627-631, 1974 and U.S. Pat. No.3,060,165).
Ribonucleases have also been conjugated to targeting molecules for use as immunotoxins (see Suzuki et al, nat. Biotech.17: 265-70, 1999). Exemplary ribotoxins such as alpha-sarcin and restrictocin are described in, for example, Rathore et al, Gene 190: 31-5, 1997; and Goyal and Batra, biochem.345 Pt 2: 247-54, 2000. Calicheamicin was first isolated from Micromonospora echinospora (Micromonospora echinospora) and is a member of the enediyne antitumor antibiotic family causing double strand breaks in DNA that lead to apoptosis (see, e.g., Lee et al, j.Antibiott.42: 1070-87, 1989). This drug is the toxic part of immunotoxins in clinical trials (see, e.g., Gillespie et al, Ann. Oncol. 11: 735-41, 2000).
Abrin includes toxic lectins from Abrus (Abrus precatorius). The toxic components abrin a, B, c and d have molecular weights of about 63kD to 67kD and are composed of two disulfide-linked polypeptide chains a and B. The A chain inhibits protein synthesis; the B chain (abrin-B) binds to a D-galactose residue (see Funatsu et al, Agr. biol. chem.52: 1095, 1988; and Olsnes, Methods enzymol.50: 330-.
CARs, CAR-expressing T cells, monoclonal antibodies, antigen-binding fragments thereof having specificity for one or more antigens disclosed herein can also be conjugated to a detectable marker; for example, a detectable marker that can be detected by: ELISA, spectrophotometry, flow cytometry, microscopy or diagnostic imaging techniques (e.g., Computed Tomography (CT), Computed Axial Tomography (CAT) scan, Magnetic Resonance Imaging (MRI), Nuclear Magnetic Resonance Imaging (NMRI), magnetic resonance tomography (MTR), ultrasound, fiber optics, and laparoscopy. Specific non-limiting examples of detectable markers include fluorophores, chemiluminescent agents, enzyme linkers, radioisotopes, and heavy metals or compounds (e.g., superparamagnetic iron oxide nanocrystals for detection by MRI). For example, useful detectable labels include fluorescent compounds, including fluorescein, fluorescein isothiocyanate, rhodamine, 5-dimethylamine-1-naphthalenesulfonyl chloride, phycoerythrin, lanthanide phosphors, and the like. Bioluminescent markers, such as luciferase, Green Fluorescent Protein (GFP), Yellow Fluorescent Protein (YFP), are also used. The CAR, T cell expressing the CAR, antibody or antigen binding portion thereof can also be conjugated to an enzyme that can be used for detection, such as horseradish peroxidase, beta-galactosidase, luciferase, alkaline phosphatase, glucose oxidase, and the like. When the CAR, T cell expressing the CAR, antibody or antigen binding portion thereof is conjugated to a detectable enzyme, it can be detected by adding additional reagents used by the enzyme to produce a discernible reaction product. For example, when the reagent horseradish peroxidase is present, the addition of hydrogen peroxide and diaminobenzidine produces a visually detectable colored reaction product. The CAR, T cell expressing the CAR, antibody, or antigen binding portion thereof can also be conjugated to biotin and detected by indirectly measuring avidin or streptavidin binding. It should be noted that avidin may itself be conjugated to an enzyme or fluorescent label.
The CAR, the T cell expressing the CAR, the antibody, or antigen binding portion thereof can be conjugated to a paramagnetic agent (e.g., gadolinium). Paramagnetic agents (e.g., superparamagnetic iron oxides) are also used as labels. Antibodies can also be conjugated to lanthanides (e.g., europium and dysprosium) and manganese. The antibody or antigen-binding fragment may also be labeled with a predetermined polypeptide epitope (e.g., a leucine zipper pair sequence, a binding site for a second antibody, a metal binding domain, an epitope tag) that is recognized by a second reporter.
The CAR, T cell expressing the CAR, antibody, or antigen binding portion thereof can also be conjugated to a radiolabeled amino acid. Radiolabels may be used for both diagnostic and therapeutic purposes, for example, radiolabels may be used to detect one or more antigens and antigen-expressing cells disclosed herein by x-ray, emission spectroscopy or other diagnostic techniques. In addition, the radioactive label can be used therapeutically as a toxin to treat a tumor in a subject, for example, to treat neuroblastoma. Some examples of labels for polypeptides include, but are not limited to, the following radioisotopes or radionucleotides:3H、14C、15N、35S、90Y、99Tc、111In、125I、131I。
methods for detecting such detectable markers are well known to those skilled in the art. Thus, for example, the radiolabel may be detected using a film or scintillation counter and the fluorescent marker may be detected using a photodetector to detect the emitted illumination. Enzyme labels are typically detected by providing a substrate to the enzyme and detecting the reaction product produced by the action of the enzyme on the substrate, and colorimetric labels are detected by simply visualizing the colored label.
D. Nucleotides, expression, vectors and host cells
One embodiment of the invention also provides a nucleic acid comprising a nucleotide sequence encoding any of the CARs, antibodies, or antigen-binding portions thereof (including functional portions and functional variants thereof) described herein. The nucleic acid of the invention may comprise a nucleotide sequence encoding any of the leader sequences, antigen binding domains, transmembrane domains and/or intracellular T cell signaling domains described herein.
In some embodiments, the nucleotide sequence may be codon modified. Without being bound by a particular theory, it is believed that codon optimization of the nucleotide sequence increases the translation efficiency of the mRNA transcript. Codon optimization of a nucleotide sequence can involve replacing a native codon with another codon that encodes the same amino acid but that can be translated by a tRNA that is more readily available in the cell, thereby increasing translation efficiency. Optimization of the nucleotide sequence may also reduce secondary mRNA structures that may interfere with translation, thereby increasing translation efficiency.
In one embodiment of the invention, the nucleic acid may comprise a codon-modified nucleotide sequence encoding the antigen binding domain of the CAR of the invention. In another embodiment of the invention, the nucleic acid may comprise a codon-modified nucleotide sequence encoding any of the CARs described herein (including functional portions and functional variants thereof).
As used herein, "nucleic acid" includes "polynucleotides," "oligonucleotides," and "nucleic acid molecules," and generally means DNA or RNA polymers, which may be single-stranded or double-stranded, synthetic, or obtained (e.g., isolated and/or purified) from a natural source; it may comprise natural, non-natural or altered nucleotides; and it may comprise natural, non-natural or altered internucleotide linkages, such as phosphoramidate linkages or phosphorothioate linkages, instead of the phosphodiester found between nucleotides of the unmodified oligonucleotide. In some embodiments, the nucleic acid does not comprise any insertions, deletions, inversions, and/or substitutions. However, as discussed herein, in some cases it may be suitable for the nucleic acid to comprise one or more insertions, deletions, inversions, and/or substitutions.
A recombinant nucleic acid can be a nucleic acid having a sequence that does not occur naturally or has a sequence that has been prepared by artificially combining two otherwise isolated segments of sequence. Such artificial combination is typically achieved by chemical synthesis or, more commonly, by artificial manipulation of isolated nucleic acid fragments, e.g., by genetic engineering techniques such as those described in Sambrook et al, supra. Nucleic acids can be constructed based on chemical synthesis and/or enzymatic ligation reactions using procedures known in the art. See, e.g., Sambrook et al, supra, and Ausubel et al, supra. For example, nucleic acids can be chemically synthesized using naturally occurring nucleotides or differently modified nucleotides designed to increase the biological stability of the molecule or to increase the physical stability of the diad formed upon hybridization (e.g., phosphorothioate derivatives and acridine substituted nucleotides). Some examples of modified nucleotides that can be used to generate nucleic acids include, but are not limited to, 5-fluorouracil, 5-bromouracil, 5-chlorouracil, 5-iodouracil, hypoxanthine, xanthine, 4-acetylcytosine, 5- (carboxyhydroxymethyl) uracil, 5-carboxymethylaminomethyl-2-thiouridine, 5-carboxymethylaminomethyluracil, dihydrouracil, β -D-galactosyltetraoside (queosine), inosine, N6-isopentenyladenine, 1-methylguanine, 1-methylinosine, 2-dimethylguanine, 2-methyladenine, 2-methylguanine, 3-methylcytosine, 5-methylcytosine, N6-substituted adenine, 7-methylguanine, 5-methylaminomethyluracil, 5-methoxyaminomethyl-2-thiouracil, β -D-mannosylbousine, 5' -methoxycarboxymethyluracil, 5-methoxyuracil, 2-methylthio-N6-isopentenyladenine, uracil-5-hydroxyacetic acid (v), wybutoxoside (wybutoxosine), pseudouracil, boudouside, 2-thiocytosine, 5-methyl-2-thiouracil, 4-thiouracil, 5-methyluracil, uracil-5-oxyacetic acid methyl ester, 3- (3-amino-3-N-2-carboxypropyl) uracil and 2, 6-diaminopurine. Alternatively, one or more nucleic acids of the invention may be purchased from companies, such as Integrated DNA Technologies (Coralville, IA, USA).
The nucleic acid may comprise any isolated or purified nucleotide sequence encoding any CAR or functional portion or functional variant thereof. Alternatively, the nucleotide sequence may comprise a degenerate nucleotide sequence or a combination of degenerate sequences of any sequence.
An embodiment also provides an isolated or purified nucleic acid comprising a nucleotide sequence that is complementary to a nucleotide sequence of any of the nucleic acids described herein or a nucleotide sequence that hybridizes under stringent conditions to a nucleotide sequence of any of the nucleic acids described herein.
Nucleotide sequences that hybridize under stringent conditions can hybridize under high stringency conditions. By "high stringency conditions" is meant that a nucleotide sequence specifically hybridizes to a target sequence (the nucleotide sequence of any of the nucleic acids described herein) in an amount that is detectably stronger than non-specific hybridization. High stringency conditions include conditions that can distinguish polynucleotides having exactly complementary sequences, or polynucleotides that contain only a few discrete mismatches, from random sequences that occasionally have several small regions (e.g., 3 to 10 bases) that match the nucleotide sequence. Such small regions of complementarity are more easily melted than full-length complements having 14 to 17 bases or more, and high stringency hybridization makes them readily distinguishable. Relatively high stringency conditions can include, for example, low salt and/or high temperature conditions, such as provided by about 0.02M to 0.1M NaCl, or equivalent, at a temperature of about 50 ℃ to 70 ℃. Such high stringency conditions allow for few, if any, mismatches between the nucleotide sequence and the template or target strand, and are particularly suitable for detecting expression of any of the CARs of the invention. It is generally understood that conditions can be made more stringent by the addition of increasing amounts of formamide.
Also provided are nucleic acids comprising a nucleotide sequence that is at least about 70% or higher, e.g., about 80%, about 90%, about 91%, about 92%, about 93%, about 94%, about 95%, about 96%, about 97%, about 98%, or about 99% identical to any of the nucleic acids described herein.
In one embodiment, the nucleic acid may be incorporated into a recombinant expression vector. In this regard, one embodiment provides a recombinant expression vector comprising any nucleic acid. For the purposes herein, the term "recombinant expression vector" means a genetically modified oligonucleotide or polynucleotide construct that allows a host cell to express an mRNA, protein, polypeptide, or peptide when the construct comprises a nucleotide sequence encoding the mRNA, protein, polypeptide, or peptide and the vector is contacted with the cell under conditions sufficient for the mRNA, protein, polypeptide, or peptide to be expressed within the cell. The carrier as a whole is not naturally occurring.
However, portions of the vector may be naturally occurring. Recombinant expression vectors may comprise any type of nucleotide, including but not limited to DNA and RNA, which may be single-or double-stranded, synthetic or partially obtained from natural sources, and which may comprise natural, non-natural or altered nucleotides. Recombinant expression vectors may contain naturally occurring or non-naturally occurring internucleotide linkages, or both types of linkages. Preferably, the non-naturally occurring or altered nucleotides or internucleotide linkages do not prevent transcription or replication of the vector.
In one embodiment, the recombinant expression vector may be any suitable recombinant expression vector and may be used to transform or transfect any suitable host cell. Suitable vectors include those designed for propagation and amplification or for expression or both, such as plasmids and viruses. The vector may be selected from the pUC series (Fermentas Life Sciences, Glen Burnie, Md.), pBluescript series (Stratagene, LaJolla, Calif.), pET series (Novagen, Madison, Wis.), pGEX series (Pharmacia Biotech, Uppsala, Sweden), and pEX series (Clontech, Palo Alto, Calif.).
Phage vectors such as1.λ Zapii (Stratagene), EMBL4 and λ NMI 149. Some examples of plant expression vectors include pBIOl, pBI101.2, pBHOl.3, pBI121, and pBIN19 (Clontech). Some examples of animal expression vectors include pEUK-Cl, pMAM, and pMAMneo (Clontech). The recombinant expression vector may be a viral vector, such as a retroviral vector or a lentiviral vector. Lentiviral vectors are vectors derived from at least a portion of the lentiviral genome, including in particular self-inactivating lentiviral vectors such as Milone et al, mol. ther.17 (8): 1453 and 1464 (2009). Further examples of lentiviral vectors that can be used clinically include, for example, but are not limited to, the lentivector.rtm. gene delivery technology from Oxford biomedical plc, the lentimax.tm. vector system from Lentigen, and the like. Non-clinical types of lentiviral vectors are also available and known to those skilled in the art.
A variety of transfection techniques are well known in the art (see, e.g., Graham et al, Virology, 52: 456-467 (1973); Sambrook et al, supra; Davis et al, Basic Methods in Molecular Biology, Elsevier (1986); and Chu et al, Gene, 13: 97 (1981)).
Transfection methods include calcium phosphate co-precipitation (see, e.g., Graham et al, supra), direct microinjection into cultured cells (see, e.g., Capecchi, Cell, 22: 479-488(1980)), electroporation (see, e.g., Shigekawa et al, BioTechniques, 6: 742-751(1988)), liposome-mediated gene transfer (see, e.g., Mannino et al, BioTechniques, 6: 682-690(1988)), lipid-mediated transduction (see, e.g., Feigner et al, Proc. Natl. Acad. Sci. USA, 84: 7413-7417(1987)), and nucleic acid delivery using high-speed microprojectiles (see, e.g., Klein et al, Nature, 327: 70-73 (1987)).
In one embodiment, recombinant expression vectors can be prepared using standard recombinant DNA techniques, for example, as described in Sambrook et al, supra, and Ausubel et al, supra. Circular or linear expression vector constructs can be prepared to contain replication systems that are functional in prokaryotic or eukaryotic host cells. Replication systems can be derived from, for example, ColEl, 2 μ plasmid, λ, SV40, bovine papilloma virus, and the like.
Recombinant expression vectors can contain regulatory sequences, such as transcription and translation initiation and termination codons, which are specific for the type of host cell (e.g., bacterial, fungal, plant, or animal) into which the vector is to be introduced, as the case may be, and with regard to whether the vector is DNA-based or RNA-based. The recombinant expression vector may contain restriction sites to facilitate cloning.
The recombinant expression vector may comprise one or more marker genes that allow for the selection of transformed or transfected host cells. Marker genes include biocide resistance, such as antibiotics, heavy metal resistance, and the like; complementation of prototrophy in an auxotrophic host, and the like. Suitable marker genes for use in the expression vectors of the invention include, for example, the neomycin/G418 resistance gene, the hygromycin resistance gene, the histidinol resistance gene, the tetracycline resistance gene, and the ampicillin resistance gene.
The recombinant expression vector may comprise a native or non-native promoter operably linked to a nucleotide sequence encoding a CAR (including functional portions and functional variants thereof) or to a nucleotide sequence complementary or hybridizing to a nucleotide sequence encoding a CAR. The choice of promoter (e.g., strong, weak, inducible, tissue-specific, and development-specific) is within the ordinary skill of the artisan. Similarly, combinations of nucleotide sequences and promoters are also within the skill of the artisan. The promoter may be a non-viral promoter or a viral promoter, such as the Cytomegalovirus (CMV) promoter, the SV40 promoter, the RSV promoter, or a promoter found in the long terminal repeats of murine stem cell viruses.
Recombinant expression vectors can be designed for transient expression, for stable expression, or for both. In addition, recombinant expression vectors can be made for constitutive expression or for inducible expression.
In addition, recombinant expression vectors can be prepared to include suicide genes. The term "suicide gene" as used herein refers to a gene that causes the death of a cell that expresses the suicide gene. The suicide gene may be the following gene: which confers sensitivity to the agent, e.g., a drug, to cells expressing the gene and causes cell death when the cells are contacted or exposed to the agent. Suicide genes are known in the art (see, e.g., suide Gene Therapy: Methods and Reviews, Springer, Caroline J. (Cancer Research UK Centre for Cancer Therapeutics at the Institute of Cancer Research, Sutton, Surrey, UK), Humana Press, 2004) and include, e.g., Herpes Simplex Virus (HSV) Thymidine Kinase (TK) Gene, cytosine deaminase, purine nucleoside phosphorylase, and nitroreductase.
One embodiment also provides a host cell comprising any of the recombinant expression vectors described herein. The term "host cell" as used herein refers to any type of cell that may comprise a recombinant expression vector of the invention. The host cell may be a eukaryotic cell, such as a plant, animal, fungus or algae, or may be a prokaryotic cell, such as a bacterium or protozoa. The host cell may be a cultured cell or a primary cell, i.e. isolated directly from an organism (e.g. a human). The host cell may be an adherent cell or a suspension cell, i.e., a cell grown in suspension. Suitable host cells are known in the art and include, for example, DH5a escherichia coli (e.coli) cells, chinese hamster ovary cells, monkey VERO cells, COS cells, HEK293 cells, and the like. For the purpose of amplifying or replicating the recombinant expression vector, the host cell may be a prokaryotic cell, such as a DH5a cell. For the purpose of producing the recombinant CAR, the host cell can be a mammalian cell. The host cell may be a human cell. While the host cell may be of any cell type, may be derived from any type of tissue, and may be at any developmental stage, the host cell may be a Peripheral Blood Lymphocyte (PBL) or a Peripheral Blood Mononuclear Cell (PBMC). The host cell may be a T cell.
For the purposes herein, a T cell may be any T cell, e.g., a cultured T cell, e.g., a primary T cell, or a T cell from a cultured T cell line, e.g., Jurkat, SupT1, etc., or a T cell obtained from a mammal. If obtained from a mammal, T cells can be obtained from a number of sourcesSources are obtained, including but not limited to, blood, bone marrow, lymph nodes, thymus, or other tissue or fluid. T cells may also be enriched or purified. The T cell may be a human T cell. The T cell may be a T cell isolated from a human. The T cells may be any type of T cell and may be at any stage of development, including but not limited to CD4+/CD8+Double positive T cell, CD4+Helper T cells (e.g. Th1 and Th2 cells), CD8+T cells (e.g., cytotoxic T cells), tumor infiltrating cells, memory T cells, memory stem cells (i.e., Tscm), naive T cells, and the like. The T cell may be CD8+T cells or CD4+T cells.
In one embodiment, the CARs described herein can be used in suitable non-T cells. Such cells are those with immune effector functions, such as, for example, NK cells and T-like cells produced by pluripotent stem cells.
One embodiment also provides a cell population comprising at least one host cell described herein. The cell population can be a heterogeneous population comprising host cells comprising any of the recombinant expression vectors and at least one other cell, e.g., a host cell (e.g., a T cell) that does not comprise any recombinant expression vector or a cell other than a T cell, e.g., a B cell, a macrophage, a neutrophil, a red blood cell, a liver cell, an endothelial cell, an epithelial cell, a muscle cell, a brain cell, etc. Alternatively, the population of cells can be a substantially homogeneous population, wherein the population comprises (e.g., consists essentially of) host cells comprising the recombinant expression vector. The population can also be a clonal population of cells, wherein all cells in the population are clones of a single host cell comprising the recombinant expression vector, such that all cells in the population comprise the recombinant expression vector. In one embodiment of the invention, the cell population is a clonal population comprising host cells comprising a recombinant expression vector, as described herein.
The CAR (including functional portions and variants thereof), nucleic acid, recombinant expression vector, host cell (including populations thereof), and antibody (including antigen binding portions thereof) can be isolated and/or purified. For example, a purified (or isolated) host cell preparation is one in which the host cell is more pure than the cell in its natural environment in vivo. Such host cells can be produced, for example, by standard purification techniques. In some embodiments, a preparation of host cells is purified such that the host cells represent at least about 50%, e.g., at least about 70%, of the total cellular content of the preparation. For example, the purity can be at least about 50%, can be greater than about 60%, about 70%, or about 80%, or can be about 100%.
E. Method of treatment
It is contemplated that the CARs disclosed herein can be used in methods of treating or preventing a disease in a mammal. In this regard, one embodiment provides a method of treating or preventing cancer in a mammal comprising administering to the mammal a CAR, a nucleic acid, a recombinant expression vector, a host cell, a population of cells, an antibody and/or antigen-binding portion thereof, and/or a pharmaceutical composition in an amount effective to treat or prevent cancer in the mammal.
One embodiment further comprises lymphodepletion (lymphodeplate) of the mammal prior to administration of the CAR disclosed herein. Some examples of lymphocyte clearance include, but may not be limited to, non-myeloablative lymphocyte clearance chemotherapy, systemic irradiation, and the like.
For the purposes of the method in which the host cell or population of cells is administered, the cells may be mammalian allogeneic or autologous cells. Preferably, the cells are autologous to the mammal. As used herein, allogenic means any material that is derived from a different animal of the same species as the individual into which it is introduced. When the genes of one or more loci are not identical, two or more individuals are considered allogeneic to each other. In some aspects, allogeneic material from individuals of the same species may be sufficiently genetically dissimilar to interact antigenically. As used herein, "autologous" means any material that originates from the same individual as the individual into which the material is later reintroduced.
The mammal referred to herein may be any mammal. The term "mammal" as used herein refers to any mammal, including but not limited to mammals of the order rodentia, such as mice and hamsters; and mammals of the order lagomorpha, such as rabbits. The mammal may be from the order carnivora, including felines (felines) and canines (canines). The mammal may be from the order artiodactyla, including bovidae (cattle) and swine (pig); or of the order perssodactyla, including equine (horse). The mammal may be from the order primates, ceboids or simoids (monkeys); or of the order simianidae (human and ape). Preferably, the mammal is a human.
With respect to the method, the cancer may be any cancer, including any of the following: acute lymphocytic cancer, acute myelogenous leukemia, alveolar rhabdomyosarcoma, bladder cancer (e.g., bladder cancer), bone cancer, brain cancer (e.g., medulloblastoma), breast cancer, anal canal cancer, or anorectal cancer, eye cancer, intrahepatic bile duct cancer, joint cancer, neck cancer, gall bladder cancer, or pleural cancer, nasal cavity cancer, or middle ear cancer, oral cavity cancer, vulval cancer, chronic lymphocytic leukemia, chronic myelogenous cancer, colon cancer, esophageal cancer, cervical cancer, fibrosarcoma, gastrointestinal carcinoid tumors, head and neck cancer (e.g., head and neck squamous cell carcinoma), hodgkin's lymphoma, hypopharynx cancer, kidney cancer, larynx cancer, leukemia, liquid tumor, liver cancer, lung cancer (e.g., non-small cell lung cancer and lung adenocarcinoma), lymphoma, mesothelioma, mastocytoma, melanoma, multiple myeloma, nasopharyngeal cancer, non-hodgkin's lymphoma, B-chronic lymphocytic leukemia, colon cancer, cervical cancer, Hairy cell leukemia, Acute Lymphoblastic Leukemia (ALL) and Burkitt's lymphoma, ovarian cancer, pancreatic cancer, peritoneal cancer, omental and mesenteric cancer, pharyngeal cancer, prostate cancer, rectal cancer, renal cancer, skin cancer, small intestine cancer, soft tissue cancer, solid tumor, synovial sarcoma, gastric cancer, testicular cancer, thyroid cancer, and ureteral cancer.
The terms "treatment" and "prevention" and words derived therefrom as used herein do not necessarily mean 100% or complete treatment or prevention. Rather, there are varying degrees of treatment or prevention that one of ordinary skill in the art would consider to have potential benefit or therapeutic effect. In this aspect, the method can provide any amount or any level of cancer treatment or prevention in the mammal.
In addition, the treatment or prevention provided by the methods can include treating or preventing one or more conditions or symptoms of a disease being treated or prevented (e.g., cancer). In addition, for purposes herein, "preventing" may encompass delaying the onset of the disease or a symptom or condition thereof.
Another embodiment provides a method of detecting the presence of cancer in a mammal comprising: (a) contacting a sample comprising one or more cells from a mammal with a CAR, a nucleic acid, a recombinant expression vector, a host cell, a population of cells, an antibody and/or antigen-binding portion thereof, or a pharmaceutical composition, thereby forming a complex; (b) and detecting the complex, wherein detection of the complex is indicative of the presence of cancer in the mammal.
The sample may be obtained by any suitable method (e.g., biopsy or necropsy). Biopsy is the removal of tissue and/or cells from an individual. Such removal may be for the purpose of collecting tissue and/or cells from an individual for performing an experiment on the removed tissue and/or cells. The experiment may include an experiment to determine whether an individual has suffered from and/or has suffered from a particular disorder or disease state. The condition or disease may be, for example, cancer.
For one embodiment of a method of detecting the presence of a proliferative disorder (e.g., cancer) in a mammal, the sample comprising cells of the mammal can be a sample comprising whole cells, whole cell lysates, or fractions of whole cell lysates (e.g., nuclear or cytoplasmic fractions, whole protein fractions, or nucleic acid fractions). If the sample comprises whole cells, the cells may be any cells of the mammal, for example cells of any organ or tissue, including blood cells or endothelial cells.
For mammals, the contacting may occur in vitro or in vivo. Preferably, the contacting is in vitro.
In addition, detection of the complex can be performed by any number of means known in the art. For example, a CAR disclosed herein, a polypeptide, a protein, a nucleic acid, a recombinant expression vector, a host cell, a population of cells, or an antibody or antigen-binding portion thereof described herein can be labeled with a detectable label, such as a radioisotope, a fluorophore (e.g., Fluorescein Isothiocyanate (FITC), Phycoerythrin (PE)), an enzyme (e.g., alkaline phosphatase, horseradish peroxidase), and an elemental particle (e.g., gold particle) as disclosed above.
Methods of testing the CAR's ability to recognize target cells and antigen specificity are known in the art. For example, Clay et al, j.immunol, 163: 507-513(1999) teaches a method of measuring the release of cytokines such as interferon- γ, granulocyte/monocyte colony stimulating factor (GM-CSF), tumor necrosis factor a (TNF-a), or interleukin 2 (IL-2). Furthermore, CAR function can be assessed by measuring cellular cytotoxicity, e.g., Zhao et al, j.immunol.174: 4415 as described in 4423 (2005).
Another embodiment provides the use of a CAR, a nucleic acid, a recombinant expression vector, a host cell, a population of cells, an antibody or antigen-binding portion thereof, and/or a pharmaceutical composition of the invention for treating or preventing a proliferative disorder (e.g., cancer) in a mammal. The cancer may be any cancer described herein.
Any method of administration may be used for the disclosed therapeutic agents, including topical and systemic administration. For example, topical, oral, intravascular (e.g., intravenous), intramuscular, intraperitoneal, intranasal, intradermal, intrathecal, and subcutaneous administration may be used. The particular mode of administration and dosage regimen will be selected by the attending clinician in view of the particular circumstances of the case (e.g., the subject, the disease state involved, and whether the treatment is prophylactic). In cases where more than one agent or composition is administered, one or more routes of administration may be used; for example, the chemotherapeutic agent may be administered orally and the antibody or antigen-binding fragment or conjugate or composition may be administered intravenously. The method of administration includes injection, in which case the CAR, CAR T cell, conjugate, antibody, antigen-binding fragment or composition is provided in a non-toxic pharmaceutically acceptable carrier such as: water, saline, ringer's solution, dextrose solution, 5% human serum albumin, fixed oils, ethyl oleate, or liposomes. In some embodiments, topical administration of the disclosed compounds can be used, for example, by applying an antibody or antigen-binding fragment to an area of tissue from which a tumor has been removed, or an area suspected of being predisposed to tumorigenesis. In some embodiments, sustained intratumoral (or peritumoral) release of a pharmaceutical formulation comprising a therapeutically effective amount of an antibody or antigen-binding fragment may be beneficial. In other examples, the conjugate is topically applied to the cornea as an eye drop, or intravitreally applied to the eye.
The disclosed therapeutic agents can be formulated in unit dosage forms suitable for single administration of precise dosages. In addition, the disclosed therapeutic agents may be administered in a single dose or in a multiple dose regimen. The multiple dose regimen is the following regimen: wherein the primary course of treatment may have more than one individual dose, for example 1 to 10 doses, followed by administration of further doses at subsequent intervals as required to maintain or potentiate the effect of the composition. Treatment may involve a daily dose or multiple daily doses of the compound over a period of days to months or even years. Thus, the dosage regimen will also be determined based at least in part on the particular needs of the subject to be treated and will depend upon the judgment of the administering physician.
A typical dose of antibody or conjugate may be from about 0.01mg/kg to about 30mg/kg, for example from about 0.1mg/kg to about 10 mg/kg.
In some specific examples, a therapeutic composition comprising one or more conjugates, antibodies, compositions, CARs, CAR T cells, or additional agents is administered to a subject based on a multiple daily dosing regimen (e.g., at least 2 consecutive days, 10 consecutive days, etc.), e.g., for a period of weeks, months, or years. In one example, the conjugate, antibody, composition, or additional agent is administered to the subject for a period of at least 30 days, such as at least 2 months, at least 4 months, at least 6 months, at least 12 months, at least 24 months, or at least 36 months.
In some embodiments, the disclosed methods comprise providing surgery, radiation therapy, and/or chemotherapy to a subject in combination (e.g., sequentially, substantially simultaneously, or simultaneously) with the disclosed antibody, antigen-binding fragment, conjugate, CAR, or CAR-expressing T cell. Such agents and methods of treatment and therapeutic dosages are known to those skilled in the art and can be determined by the skilled clinician. The preparation and dosing regimen for the additional agent may be used according to the manufacturer's instructions or as determined empirically by the skilled artisan. Formulations and dosing regimens for such Chemotherapy are also described in Chemotherapy Service, (1992) editors, m.c. perry, Williams & Wilkins, Baltimore, Md.
In some embodiments, the combination therapy may comprise administering to the subject a therapeutically effective amount of an additional cancer inhibitor. Non-limiting examples of additional therapeutic agents that may be used in combination therapy include microtubule binding agents, DNA intercalating or crosslinking agents, DNA synthesis inhibitors, inhibitors of DNA and RNA transcription, antibodies, enzymes, enzyme inhibitors, gene modulators, and angiogenesis inhibitors. These agents (which are administered in therapeutically effective amounts) and treatments may be used alone or in combination. For example, any suitable anti-cancer or anti-angiogenic agent can be administered in combination with a CAR, CAR-T cell, antibody, antigen-binding fragment, or conjugate disclosed herein. Methods and therapeutic dosages of such agents are known to those of skill in the art and can be determined by the skilled clinician.
Additional chemotherapeutic agents include, but are not limited to, alkylating agents such as nitrogen mustards (e.g., chlorambucil, chloramine (chlormethine), cyclophosphamide, ifosfamide, and melphalan), nitrosoureas (e.g., carmustine, fotemustine, lomustine, and streptozocin), platinum compounds (e.g., carboplatin, cisplatin, oxaliplatin, and BBR3464), busulfan, dacarbazine, mechlorethamine, procarbazine, temozolomide, thiotepa, and uracil mustard; antimetabolites such as folic acid (e.g., methotrexate, pemetrexed, and raltitrexed), purines (e.g., cladribine, clofarabine, fludarabine, mercaptopurine, and rauvolvuline (tioguanine)), pyrimidines (e.g., capecitabine), cytarabine, fluorouracil, and gemcitabine; plant alkaloids, such as podophyllum (e.g., etoposide and teniposide), taxanes (e.g., docetaxel and paclitaxel), vinblastines (e.g., vinblastine, vincristine, vindesine, and vinorelbine); cytotoxic/antitumor antibiotics, such as members of the anthracycline family (e.g., daunorubicin, doxorubicin, epirubicin, idarubicin, mitoxantrone, and valrubicin), bleomycin, rifampin, hydroxyurea (hydroxyurea), and mitomycin; topoisomerase inhibitors, such as topotecan and irinotecan; monoclonal antibodies, such as alemtuzumab, bevacizumab, cetuximab, gemtuzumab ozogamicin, rituximab, panitumumab, pertuzumab, and trastuzumab; photosensitizers such as aminolevulinic acid, methyl aminolevulinic acid, porfimer sodium, and verteporfin; and other agents, such as alitretinoin, altretamine, amsacrine, anagrelide, arsenic trioxide, asparaginase, acitinib, bexarotene, bevacizumab, bortezomib, celecoxib, dinebin (dilueukin diftitox), erlotinib, estramustine, gefitinib, hydroxyurea (hydroxyarbamide), imatinib, lapatinib, pazopanib, pentostatin, masopropiol, mitotane, pemetrexed, tamoxifen, sorafenib, sunitinib, vemurafinib, vandetanib, and retinoic acid. The choice of such agents and therapeutic dosages are known to those skilled in the art and can be determined by the skilled clinician.
Combination therapy can provide a synergistic effect and prove synergistic, i.e., the effect achieved when the active ingredients are used together is greater than the sum of the effects produced by the compounds used alone. When the active ingredients are: (1) co-formulated in a combined unit dose formulation and administered or delivered simultaneously; (2) delivered alternately or concurrently in separate formulations; or (3) by other protocols, a synergistic effect may be obtained. When delivered alternately, a synergistic effect may be obtained when the compounds are administered or delivered sequentially, for example sequentially in separate syringes by different injections. Generally, during alternation, the effective doses of each active ingredient are administered sequentially, i.e. one after the other, whereas in combination therapy the effective doses of two or more active ingredients are administered together.
In one embodiment, an effective amount of an antibody or antigen-binding fragment or conjugate thereof that specifically binds to one or more antigens disclosed herein is administered to a subject having a tumor after an anti-cancer treatment. The immune complex is detected after a sufficient amount of time has elapsed to allow the administered antibody or antigen-binding fragment or conjugate to form an immune complex with the antigen expressed on the corresponding cancer cell. The presence (or absence) of the immune complex indicates the effectiveness of the treatment. For example, an increase in immune complexes compared to controls taken prior to treatment indicates that the treatment is not effective, whereas a decrease in immune complexes compared to controls taken prior to treatment indicates that the treatment is effective.
F. Biological medicine composition
Provided herein are biopharmaceutical or biologicai compositions (hereinafter "compositions") for gene therapy, immunotherapy, and/or cell therapy comprising one or more of the disclosed CARs, or CAR-expressing T cells, antibodies, antigen-binding fragments, conjugates, CARs, or CAR-expressing T cells, in a carrier (e.g., a pharmaceutically acceptable carrier) that specifically binds to one or more of the antigens disclosed herein. The compositions may be prepared in unit dosage form for administration to a subject. The amount and timing of administration is determined by the treating clinician to achieve the desired result. The compositions can be formulated for systemic (e.g., intravenous) or topical (e.g., intratumoral) administration. In one example, the disclosed CARs, or T cells expressing CARs, antibodies, antigen-binding fragments, conjugates are formulated for parenteral administration, e.g., intravenous administration. Compositions comprising a CAR disclosed herein, or a T cell, conjugate, antibody or antigen-binding fragment expressing a CAR, are useful, for example, in the treatment and detection of tumors, such as, but not limited to, neuroblastoma. In some examples, the compositions can be used for the treatment or detection of cancer. Compositions comprising a CAR, or a T cell, conjugate, antibody or antigen-binding fragment expressing a CAR as disclosed herein are also useful, for example, in the detection of pathological angiogenesis.
Compositions for administration may include a solution of the CAR, or T cells expressing the CAR, conjugates, antibodies, or antigen-binding fragments, dissolved in a pharmaceutically acceptable carrier (e.g., an aqueous carrier). A variety of aqueous carriers can be used, such as buffered saline and the like. These solutions are sterile and generally free of undesirable substances. These compositions may be sterilized by conventional, well-known sterilization techniques. These compositions may contain pharmaceutically acceptable auxiliary substances as necessary to approximate physiological conditions, such as pH adjusting and buffering agents, toxicity adjusting agents, auxiliary agents and the like, for example, sodium acetate, sodium chloride, potassium chloride, calcium chloride, sodium lactate and the like. The concentration of CAR, or T cells expressing the CAR, antibody or antigen binding fragment or conjugate in these formulations can vary widely and will be selected primarily based on fluid volume, viscosity, body weight, etc., according to the particular mode of administration selected and the needs of the subject. The actual methods of preparing such dosage forms for gene therapy, immunotherapy and/or cell therapy are known or will be apparent to those skilled in the art.
Typical compositions for intravenous administration comprise about 0.01mg/kg to about 30mg/kg of the antibody or antigen-binding fragment or conjugate per subject per day (or a corresponding dose of CAR comprising the antibody or antigen-binding fragment, or a T cell expressing the CAR, conjugate). The actual methods for preparing the administrable compositions are known or apparent to those skilled in the art and are described in more detail in publications such as Remington's Pharmaceutical Science, 19 th edition, Mack Publishing Company, Easton, PA (1995).
The CAR, or T cell expressing the CAR, antibody, antigen binding fragment or conjugate can be provided in lyophilized form and rehydrated with sterile water prior to administration, but it is also provided in a sterile solution of known concentration. The CAR, or the CAR-expressing T cells, antibody or antigen-binding fragment or conjugate solution is then added to an infusion bag containing 0.9% sodium chloride (USP) and in some cases administered at a dose of 0.5mg/kg to 15mg/kg body weight. Considerable experience is available in the art in the administration of antibodies or antigen-binding fragments and conjugate drugs; for example since 1997Antibody drugs have been sold in the united states since their approval. CAR, or T cells, antibodies, antigens expressing CARThe binding fragments and conjugates thereof may be administered by slow infusion rather than as an intravenous bolus or bolus. In one example, a higher loading dose is administered followed by a maintenance dose at a lower level. For example, an initial loading dose of 4mg/kg of antibody or antigen-binding fragment (or a corresponding dose of conjugate comprising antibody or antigen-binding fragment) may be infused over a period of about 90 minutes, followed by a weekly maintenance dose of 2mg/kg over a period of 30 minutes for 4 to 8 weeks if the previous dose is well tolerated.
The controlled release parenteral formulation can be prepared as an implant, an oily injection or as a particulate system. For a summary of protein delivery systems, see Banga, a.j., Therapeutic Peptides and Proteins: formulation, Processing, and Delivery Systems, technical Publishing Company, Inc., Lancaster, PA, (1995). Particle systems include microspheres, microparticles, microcapsules, nanocapsules, nanospheres, and nanoparticles. Microcapsules contain a therapeutic protein (e.g., a cytotoxin or drug) as the central core. In the microspheres, the therapeutic agent is dispersed throughout the particle. Particles, microspheres and microcapsules of less than about 1 μm are generally referred to as nanoparticles, nanospheres and nanocapsules, respectively. The diameter of the capillary is about 5 μm so that only nanoparticles are administered intravenously. The microparticles are typically about 100 μm in diameter and are administered subcutaneously or intramuscularly. See, e.g., Kreuter, J., Colloidal Drug Delivery Systems, J.Kreuter, eds., Marcel Dekker, Inc., New York, NY, pp.219 to 342 (1994); and Tice & Tabibi, treat on Controlled Drug Delivery, A.Kydonieus editors, Marcel Dekker, Inc.New York, NY, pages 315 to 339 (1992).
The polymers can be used for ionic controlled release of a CAR disclosed herein, or a T cell expressing the CAR, an antibody or antigen binding fragment or conjugate composition. A variety of degradable and non-degradable polymeric matrices for controlled drug delivery are known in the art (Langer, Account Chem. Res.26: 537. sup. 542, 1993). For example, block copolymer poloxamer 407 exists as a viscous but mobile liquid at low temperature, but forms a semi-solid gel at body temperature. It has been shown to be an effective vehicle for the formulation and sustained delivery of recombinant interleukin-2 and urease (Johnston et al, pharm. Res.9: 425-434, 1992; and Pec et al, J.Parent. Sci. Tech.44 (2): 58-65, 1990). Alternatively, hydroxyapatite has been used as a microcarrier for the controlled release of proteins (Ijntema et al, int.J.pharm.112: 215-224, 1994). In another aspect, liposomes are used for controlled release and Drug targeting of lipid encapsulated drugs (Betageri et al, Liposome Drug Delivery Systems, technical Publishing Co., Inc., Lancaster, PA (1993)). Many additional systems for controlled delivery of therapeutic proteins are known (see U.S. Pat. No.5,055,303; U.S. Pat. No.5,188,837; U.S. Pat. No.4,235,871; U.S. Pat. No.4,501,728; U.S. Pat. No.4,837,028; U.S. Pat. No.4,957,735; U.S. Pat. No.5,019,369; U.S. Pat. No.5,055,303; U.S. Pat. No.5,514,670; U.S. Pat. No.5,413,797; U.S. Pat. No.5,268,164; U.S. Pat. No.5,004,697; U.S. Pat. No.4,902,505; U.S. Pat. No.5,506,206; U.S. Pat. No.5,271,961; U.S. Pat. No..
G. Medicine box
In one aspect, kits for using the CARs disclosed herein are also provided. For example, the kit is used to treat a tumor in a subject, or to prepare a CAR T cell that expresses one or more CARs disclosed herein. As disclosed herein, a kit will generally comprise the disclosed antibodies, antigen-binding fragments, conjugates, nucleic acid molecules, CARs, or T cells expressing CARs. More than one of the disclosed antibodies, antigen-binding fragments, conjugates, nucleic acid molecules, CARs, or CAR-expressing T cells can be included in the kit.
The kit may comprise a container and a label or package insert on or attached to the container. Suitable containers include, for example, bottles, vials, syringes, and the like. The container may be formed from a variety of materials, such as glass or plastic. The container typically contains a composition comprising one or more of the disclosed antibodies, antigen-binding fragments, conjugates, nucleic acid molecules, CARs, or CAR-expressing T cells. In some embodiments, the container may have a sterile access port (e.g., the container may be an intravenous solution bag or a vial having a stopper pierceable by a hypodermic injection needle). The indicia or package insert indicates that the composition is used to treat a particular condition.
The marker or packaging insert will also typically include instructions for using the disclosed antibodies, antigen-binding fragments, conjugates, nucleic acid molecules, CARs, or CAR-expressing T cells, for example, in methods of treating or preventing tumors or making CAR T cells. The package insert typically includes instructions, typically included in commercial packaging for the therapeutic product, that contain information regarding the indications, usage, dosage, administration, contraindications and/or warnings associated with the use of such therapeutic products. The illustrative material may be written in electronic form (e.g., a computer diskette or compact disk) or may be visualized (e.g., a video file). The kit may also contain additional components that facilitate the particular application for which the kit is designed. Thus, for example, the kit may additionally comprise means for detecting the label (e.g.an enzyme substrate for an enzymatic label, a filter device for detecting a fluorescent label, a suitable second label (e.g.a second antibody), etc.). The kit may additionally contain buffers and other reagents normally used in the practice of the particular method. Such kits and suitable contents are well known to those skilled in the art.
Examples
The present invention is further illustrated by the following examples, which should not be construed in any way as imposing limitations upon the scope thereof. On the contrary, it is to be clearly understood that resort may be had to various other embodiments, modifications, and equivalents thereof which, after reading the description herein, may become apparent to those skilled in the art without departing from the spirit of the present invention and/or the scope of the appended claims.
Example 1 isolation of antibodies specific for CD33 from ScFv and VH repertoire displayed by fully human phage
Materials and methods:
a) generation of human phage-displayed ScFv and VH CD 33-specific antibodies
Use of a naive human ScFv (Immunity) constructed from peripheral blood B cells from 50 healthy donorsRecombinant single-chain variable fragments of globin) phage display library (approximately diverse, with 1010Species unique specificity) (z.y.zhu and d.s.dimitrov, unpublished data) and human HV (immunoglobulin heavy chain variable domain) libraries to select ScFv or VH specific for recombinant human CD 33. Will 1012Amplified libraries of individual phage-displayed ScFv or VH were incubated with 5,3 and 1 μ g of coated CD33 in 5x100- μ l volumes evenly distributed in 5 wells of a 96-well plate during the first, second and third rounds of biopanning, respectively, for two hours at room temperature. After each round of incubation, wells were washed 5 times for the first round with Phosphate Buffered Saline (PBST) containing 0.05% Tween 20 and 10 times for the following round to remove non-specifically bound phage, bound phage were mixed with TG1 competent cells for 1 hour at 37 ℃, phage were amplified from infected cells and used for the next round of biopanning. After the third biopanning round, 380 clones were randomly picked from infected TG1 cells using an automated BioRobotics BioPick colony picking System (Genomic Solutions, Ann Arbor, MI) and each inoculated into 150. mu.l of 2YT medium containing 100. mu.g/ml carbenicillin and 0.2% glucose in 96-well plates. After the bacterial culture reached an optical density of 0.5 at 600nm (OD600), the helper phage M13K07 with a multiplicity of infection (MOI) of 10 and kanamycin at 50. mu.g/ml (final concentration) were added to the medium and the plates were further incubated overnight at 30 ℃ on a shaker at 250 rpm. Phage supernatants were mixed with 3% skim milk in PBS at a 4: 1 volume ratio and used in an enzyme-linked immunosorbent assay (ELISA) to identify phage clones displaying ScFv or VH with high CD33 binding affinity. Supernatants were incubated with 50ng of coated recombinant human CD33 per well in 96-well plates for 2 hours at room temperature and washed five times with PBST (after incubation overnight at 4 ℃, blocked with 3% skim milk in PBS and washed 3 times with PBS containing 0.05% Tween 20.) and CD 33-bound phage were detected using horseradish peroxidase-conjugated goat anti-M13 antibody. After incubation with antibody, non-specifically bound antibody was removed by washing the wells and 3,3 ', 5' -Tetramethylbenzidine (TMB) substrate was added and the absorbance of the solution at 450nm was measured (a 45)0). Clones binding to CD33 with a450 > 1.0 were selected for further characterization.
b) Expression and purification of selected soluble ScFv or VH
The VH and VL of the selected clones and the VH of the domain binder were DNA sequenced and ScFv or VH with unique sequences encoded by the clones were expressed and purified as described below. Plasmids extracted from these clones were used for the transformation of HB2151 cells. Individual colonies were picked from plates containing freshly transformed cells, inoculated into 200ml 2YT medium containing 100. mu.g/ml ampicillin and 0.2% glucose, and incubated at 37 ℃ with shaking at 250 rpm. When the OD of the culture at 600nm reached 0.90, isopropyl- β -d-thiogalactopyranoside was added at a final concentration of 0.5mM, and the culture was further incubated overnight at 30 ℃. Bacterial pellets were collected after centrifugation at 8,000 Xg for 20 minutes and resuspended in PBS buffer containing 0.5mU of polymyxin B (Sigma-Aldrich, St. Louis, Mo.). After 30 min of spin incubation at 50rpm at room temperature, the resuspended pellet was centrifuged at 25,000 × g for 25 min at 4 ℃ and the supernatant was used for ScFv purification using Ni-NTA resin according to the supplier protocol (Qiagen).
c) ELISA binding assay
Diluted recombinant human CD33 in 50 μ l PBS was encapsulated overnight at 2ug/ml in 96-well plates at 4 ℃. Purified ScFv or VH (from above) with His and Flag tags were serially diluted and added to target protein coated wells. After washing, HRP-conjugated anti-Flag antibody was added at 1: 3000 dilution for 1 hour at room temperature. After washing, 3, 5, 5' -Tetramethylbenzidine (TMB) substrate was added, and after incubation at room temperature for 10 minutes, 1N H was added2SO4To stop the reaction and read the o.d. at 450m to quantify the relative ability of ScFv to bind CD 33.
As a result:
based on the results of the ELISA binding assay, four separate ScFs clones specific for recombinant human CD33 were identified and labeled as human anti-CD 33 ScFv conjugate m1033-9(ScFv9), m1033-10(ScFv10), m1033-12(ScFv12) and m1033-15(ScFv15), respectively. Two unique VH domain binders m1033-2(VH-2) and m1033-4(VH-4) were also identified from ELISA binding assays. The generation of chimeric antigen receptors expressing VH-2, VH-4, ScFv9, ScFv10, ScFv12 and ScFv15 human anti-CD 33 conjugates is outlined in example 2 below.
Example 2 expression of anti-CD 33 fully human heavy chain only Ig or scFv based binding sequences
In this example, novel fully human immunoglobulin heavy chain-only anti-CD 33 CAR T cells derived from single chain variable fragment (scFv) conjugate sequences are described. The novel anti-CD 33 CART construct has been shown to be expressed at high levels in primary human T cells, and has specificity and potent cytotoxicity and cytokine function against CD33 positive tumor cells.
Homo sapiens (Homo sapiens) CD33 (sialic acid binding to Ig-like lectin 3, SIGLEC3, SIGLEC-3, gp67, p67) is a well studied target on Acute Myeloid Leukemia (AML). The CD33 humanized antibodies (lintuzumab) and the CD33 antibody-drug conjugate (gemtuzumab or GO, Pfizer) showed some efficacy but failed to show robust therapeutic benefit in clinical trials (1.Feldman EJ et al, J Clin Oncol 2005; 23 (18): 4110-. AMG330, a CD33-CD3 bispecific T cell adaptor (BITE) (Krupka C et al, Blood 2014123: 356-365) is also being investigated. By this year GO has been reintroduced clinically with altered, much lower doses and modified protocols, but sufficient clinical data has yet to be accumulated to reevaluate the agent. Another agent currently under development, the CD33 targeted antibody-drug conjugate vadastuximab talirine (SGN-CD33A), has recently been clinically relegated in several clinical phase I/II trials due to hepatotoxicity (available on the world wide web in.
CD33 CARs were designed using CD33 binding sequences derived from immunoglobulin VH domains or full-length ScFv under the control of EF1a promoter and tested for transduction efficiency, killing function and cytokine production in vitro.
Materials and methods:
(a) cell lines
Human cell lines promyelocytic leukemia HL-60, acute lymphocytic leukemia Reh, monocytic leukemia THP-1, and myelogenous leukemia K562 cell lines were purchased from the American Tissue Culture Collection (ATCC, Manassas, Va.). The acute myeloid leukemia MOLM-14 line was obtained from the German Collection of Microorganisms and Cell Lines (DSMZ, Braunschweig Germany). The cell lines were cultured in RPMI-1640 medium (ATCC) supplemented with 10% heat-inactivated fetal bovine serum. THP-1 medium also contained 0.05% beta mercaptoethanol. Luciferase expressing subclones were generated by stable transduction of wild type leukemia cell lines with a firefly luciferase encoding lentiviral vector (Lentigen Technology, Inc., Gaithersburg, Md.) with or without GFP, followed by limiting dilution and selection of luciferase positive clones.
(b) Establishment of Chimeric Antigen Receptor (CAR) -expression vectors
The CAR antigen binding domain sequence is derived from a human anti-CD 33 ScFv or heavy chain variable fragment. The CAR T construct was generated by linking the binder sequence to the CD8a and transmembrane domain (UniProt sequence ID P01732, aa 138- "206) and then in-frame with the 4-1BB (CD137, aa 214-" 255, UniProt sequence ID Q07011) signaling domain and the CD3 zeta signaling domain (CD247, aa 52-163, reference sequence ID: NP-000725.1). For some constructs, a CD28 co-stimulatory sequence was used instead of the 4-1BB co-stimulatory sequence. In some constructs, the CD8 ligation and/or transmembrane domain is replaced with a domain derived from the TNFRSF19 protein. For some sequences, a truncated epidermal growth factor receptor (tfegfr) tag was incorporated into the CAR construct via the 2A peptide to enable labeling of transduced cells in vitro, as well as serving as a suicide switch for in vivo applications. CAR construct sequences were cloned into a third generation lentiviral plasmid backbone (Lentigen Technology inc., Gaithersburg, MD). Supernatants containing Lentiviral Vectors (LV) were generated by transient transfection of HEK 293T cells, the vectors were pelleted by centrifugation of the supernatants containing lentiviral vectors and stored at-80 ℃.
(c) Purification and transduction of primary T cells
Human primary T cells from normal donors were paired with CD4 according to the manufacturer's protocol (Miltenyi Biotec, Bergisch Gladbach, Germany)+And CD8+Cells were purified from buffy coat after immunomagnetic bead selection in TexMACS media supplemented with 40IU/ml IL-2 at 0.3X106Cell/ml to 2X106Cells/ml were cultured at CD3/CD28GMP TransAct reagent (Miltenyi Biotec) was activated and transduced with lentiviral vector encoding the CAR construct overnight in the presence of 10 μ g/ml protamine sulfate (Sigma-Aldrich, st. louis, MO) on day 2 and the medium was changed on day 4. On day 3, cultures were transferred to TexMACS medium supplemented with 200IU/ml IL-2 and propagated until harvested on days 7 to 10.
(d) Immune effector assay (CTL and cytokine)
To determine cell-mediated cytotoxicity (CTL assay), 5,000 target cells stably transduced with firefly luciferase were combined with CAR T cells at various effector/target ratios and incubated overnight. SteadyGlo reagent (Promega, Madison Wis.) was added to each well and the resulting luminescence was quantified as counts per second (sample CPS). Target-only wells (maximum CPS) and target-only wells plus 1% Tween-20 (minimum CPS) were used to determine assay range. The specific cleavage percentage was calculated as (1- (sample CPS-minimum CPS)/(maximum CPS-minimum CPS)). Supernatants of co-cultures with an E: T ratio of 10: 1 were removed and analyzed for IFN γ, TNF α and IL-2 concentrations by ELISA (eBioscience, San Diego, Calif.).
(e) Flow cytometry analysis of CAR surface expression
For cell staining, fifty thousand CAR T transduced cells were harvested from culture, washed twice in cold AutoMACS buffer supplemented with 0.5% bovine serum albumin (Miltenyi Biotec), and purified by treatment with CD33-Fc peptide (R)&D, Minneapolis, MN) and then with anti-Fc-AF 647 conjugate (Jackso)n ImmunoResearch, West Grove, Pa.) staining to detect CAR surface expression. Untransduced cells were used as negative control. Dead cells were excluded from all studies by 7AAD staining (BD Biosciences, San Jose, CA). Cells were washed twice and resuspended in 200 μ l staining buffer before quantitative analysis by flow cytometry. In thatFlow cytometry analysis was performed on a 10 analyzer (Miltenyi Biotec) and data plots were generated using FlowJo software (Ashland, OR).
(f) In vivo analysis of CAR T function
The function of CD 33-targeted CAR T cells was evaluated in vivo. 6 to 8 week old NSG mice (6 mice per group) were inoculated with 1.0x10 on day 06Individual MOLM-14CD33+AML cells. Tumor burden was determined by IVIS bioluminescence imaging on day 4, mice were randomized into groups of equal mean tumor burden, and 5.0x10 was administered on day 5 of the study6A CAR T+Cells/mouse. Regression of the tumors was determined by bioluminescence imaging on days 14, 21,28 and 35. Survival of the mice was recorded and analyzed at the end of the study. To determine the presence of CAR T and tumor cells, blood was collected from all animals on study day 19. The absolute numbers of blood CAR T cells and MOLM-14 tumor cells were determined by flow cytometry and the levels of inflammatory cytokines were measured in plasma by the MACSPlex cytokine 12 human kit (Miltenyi Biotec) following the manufacturer's protocol.
(g) Flow cytometry analysis of CAR T and tumor cells in mouse blood
For flow cytometry, 50ul of blood was collected and CAR T and MOLM-14 tumor cell numbers were analyzed. First, erythrocytes were lysed with erythrocyte lysis buffer (Miltenyi Biotec) according to the manufacturer's instructions, and human CD45 was used+,CD3+(Miltenyi Biotec) and 7-AAD (BD Biosciences, San Jose, Calif.) stained leukocytes and obtained by MACSQiant 10 flow cytometer (Miltenyi Biotec). MOLM-14-cells stably expressing the GFP reporter were detected in the B1 channel. From analysisSeven AAD positive dead cells were excluded. To facilitate direct quantification of the number of human T cells and MOLM-14 in blood, CountBright absolute counting beads (ThermoFischer Scientific, Waltham, MA) were added to each sample prior to acquisition and the corresponding absolute cell numbers were calculated according to the manufacturer's protocol.
(h) Long-term CAR T and tumor co-incubation assays
CART cell lines expressing various anti-CD 33 CAR constructs and controls were combined with tumor target HL-60 cells at effector to target ratios of 5: 1 to 0.04: 1 for 5 or 11 days. Negative controls UTD (untransduced cells), T cells alone (E: T1: 0), and T cells expressing GFP (1398) were included. At each time point, cells were stained with anti-human CD33 and CD3 antibodies and 7-AAD and taken on a macSQurant 10 flow cytometer. To determine the percentage of CAR T cells and tumor cells that survived in each case, cells were scattered forward and side by a single peak 7-AAD-、CD3+Or CD33+And a door is arranged on the upper part.
As a result:
to evaluate the novel anti-CD 33 fully human ScFv binding sequences, CAR constructs were designed incorporating either the heavy chain-only binder sequence VH-2 or VH-4 or the ScFv sequences ScFv9, ScFv10, ScFv12 or ScFv15 as the tumor antigen binding domain. In each CAR design, the tumor targeting domain was followed by a linker and transmembrane domain derived from human CD8 protein, a 4-1BB costimulatory domain, and a CD3 zeta signaling domain (table 1 below). Construct LTG1940 incorporating an ScFv binding domain derived from the sequence My96 was used as a reference control or comparator.
Table 1: list of CD 33-targeted CAR constructs
LTG1905:EF1a VH-2 CD33-CD8 TM-41BB-CD3ζ
LTG1906:EF1a VH-4 CD33-CD8TM-4-1BB-CD3ζ
LTG1936:EF1a-ScFv9-CD8TM-4-1BB-CD3ζ
LTG1937:EF1a-ScFv10-CD8TM-4-1BB-CD3ζ
LTG1938:EF1a-ScFv12-CD33 CAR-CD8TM-4-1BB-CD3ζ
LTG1939:EF1a-ScFv15-CD33 CAR-CD8TM-4-1BB-CD3ζ
LTG1940:EF1a-My96_ScFv-CD33 CAR-CD8TM-4-1BB-CD3ζ
T cells transduced with anti-CD 33 chimeric antigen receptors showed surface expression and cytolytic activity.
a) Surface expression of anti-CD 33 CAR
To evaluate the novel anti-CD 33 CARs, Lentiviral Vectors (LVs) encoding CAR constructs under the control of the human EF1a promoter were generated as described in materials and methods. Human primary T cells from two independent healthy donors were then transduced with four lentiviral vectors encoding CARs. Either untransduced cells (NTs) from the same donor or GFP-transduced cells from the same donor were used as negative controls.
T cells were activated with TransAct T cell reagents (active linker of CD3 and CD28 antigen, Miltenyi Biotec, Inc.) on day 0 of culture in the presence of IL-2 as described in materials and methods. On day 10 of culture, the expression of anti-CD 33 CAR on the surface of T cells was detected by CD33-Fc peptide followed by anti-Fc-AF 647 and analyzed by flow cytometry. The anti-CD 33 CAR construct exhibited surface CAR expression.
b) Cytolytic assay for anti-CD 33 CAR
To demonstrate the cytolytic function of the CAR T cells generated, luciferase-based killing assays were performed using HL-60-luc, MOLM-14(CD 33-high), Reh-luc and K562-luc (CD 33-low) leukemia cell lines stably expressing firefly luciferase. CART cells were combined with target cells at effector to target (E: T) ratios of 20, 10 and 5 and incubated overnight, and cell killing was then assessed by luminescence as described in materials and methods (figure 3 figure 4; figure 6 and figure 7). When tested for VH-based anti-CD 33 CARs, CAR T construct LTG1906 exhibited strong E: T ratio-dependent cytotoxicity on high CD33 HL-60-luc cell line, moderate cell lysis on lower CD 33-expressing K562 cell line, and only weak cell lysis activity of low CD33 Reh-luc cell line. Thus, cytolytic activity is directly related to CD33 expression levels in leukemia. Furthermore, the negative control GFP construct LTG1398 and NT (untransduced T cells from the same donor) had no cytolytic effect, indicating that cytotoxicity is CART-dependent. Notably, the LTG1905 CAR construct was not cytolytic in the HL-60 luc cell line, but had only weak cytolysis in the K562-luc cell line.
Likewise, construct LTG1906 produced high levels of IFN γ, TNF α and IL-2 in response to the highly CD33 positive tumor lines THP-1 and HL-60, while CAR T secreted cytokines were still at low levels when challenged with leukemia cell line K562 or Reh expressing low levels of CD33 antigen (figure 5). Interestingly, construct LTG1905, although ineffective in killing CD 33-positive HL-60 leukemia in vitro, produced very high levels of IFN γ, TNF α and IL-2, as detected by ELISA. Thus, the design of the CAR and the choice of binders is not trivial, as some binders are active in soluble IgG or ScFv format and can be expressed on the T cell surface in CAR T format, but they are inefficient in killing CD33 positive tumors.
In contrast, when ScFv anti-CD 33 CAR T cells were tested, constructs LTG1936 and LTG1939 showed robust killing activity against the high CD33 tumor cell lines HL-60 and MOLM-14, while activity against the low CD33 Reh tumor cell line was much lower and hardly detectable against the low CD 33K 562 cells (fig. 7). Surprisingly and unexpectedly, CAR constructs LTG1937 and LTG1938 were inefficient at cleaving CD33 positive tumor targets. This again demonstrates that the CAR T constructs based on antibody fragmentsIs not insignificant, as soluble antibody binding properties and/or solubility and/or multimerization properties, etc. may not translate directly into CAR function. Similar to VH-only construct 1906, scFv-based constructs 1936, 1939 and My96 scFv-based comparator construct 1940 were in the presence of high CD33+Both tumour cell lines HL-60 and MOLM14 produced high levels of IFN γ and TNF α when challenged, but at CD33Is low inThere was little cytokine induction in the presence of the cell line Reh or when CART cells were incubated alone in the absence of target cells. CAR constructs 1937, 1938, which have shown poor killing function in vitro, are also inefficient in cytokine production in response to tumor cells (data not shown). MOLM14 exhibited higher CD33 antigen density compared to cytokine induction by MOLM14 and HL60 (30,000 sites per cell in MOLM14 compared to 25,000 sites per cell in HL-60, data not shown), which corresponds to greater IFN γ and TNF α induction by MOLM14 for all anti-CD 33 constructs tested. Again, this demonstrates the antigen-specific nature of anti-CD 33 CAR activation. Unexpectedly, the induction of IL-2 was strong for CAR constructs 1906 and 1940, but moderate for CAR constructs 1936 and 1939.
Then, by contacting CAR T cells incorporating different constructs with HL-60 CD33 in culture+Tumor cells were combined at an E: T ratio of 5: 1 to 0.04: 1 for long-term co-incubation assays. Untransduced T cells UTD, GFP transduced T cells 1398 and T cells alone of E: T0.1 were used as assay controls. Cells were co-cultured for 5 days (data not shown) or 11 days, both of which showed a similar trend of HL-60 elimination for each CAR construct (fig. 9). In the negative control group (UTD and 1398), tumor cells grew rapidly and T cells disappeared, indicating that CAR-mediated T cell stimulation is required for cytolytic activity and prolonged survival of CAR T. CAR constructs 1398, 1398 that performed poorly in the overnight in vitro assay were ineffective in HL-60 killing in this long-term assay and similar to the performance of the negative control group, CAR T cells disappeared from culture and tumors persisted at all E: T ratios equal to or below 1: 1. In contrast, anti-CD 33 CAR constructs 1906, 1936 and1939 it is equally potent in CTL function as the comparator construct 1940 and successfully eliminates HL-60 tumor cells at E: T ratios as low as 0.2: 1 (FIG. 9). Thus, constructs 1906, 1936, 1939, and 1940 were selected for further evaluation in an AML in vivo model.
To facilitate comparison of the anti-CD 33-CAR constructs in vivo, a xenograft mouse model was used as described in materials and methods. Briefly, NSG mice were inoculated with MOLM-14 cells stably expressing firefly luciferase and GFP on day 0 and 500 ten thousand CAR T cells per mouse were administered on study day 5. Tumor growth kinetics were measured by IVIS bioluminescence imaging on study days 14, 21,28, 35, and CAR T function in mouse blood was assessed on study day 19.
As shown in a of figure 10, mice transplanted with MOLM-14 tumors and either untreated (TA) or administered untransduced T cell control (UTD) died of the disease by day 14 of the study. CAR constructs 1936 and 1939 exhibit partial efficacy and delay tumor growth and prolong survival. Strikingly, CAR construct 1906 and comparator construct 1940 mediated MOML-14 tumor rejection, and all animals in these groups survived to the end of the study at day 39 (a and B of fig. 10).
Blood was drawn from each animal on study day 19 to assess CAR T cell levels in blood, MOLM-14 tumor cell levels in blood, and CAR T secreted blood cytokine levels in each treatment group. Absolute CART and tumor cell numbers in blood samples were measured by flow cytometry (a of fig. 11, left panel). Although there was no significant difference in the number of CAR T cells in each group, the CAR T cell expressing construct 1906 tended to be higher than the other groups, followed by CAR comparator construct 1940. Interestingly, the T cell levels were also higher in the UTD control group containing untransduced T cells, probably due to the large number of cells initially infused in this group (8.0x 10)6Individual cells/mouse). Notably, we detected a statistically significant reduction in the number of circulating blood MOLM-14 tumor cells in all CAR T groups compared to UTD controls (fig. 11, a, right panel). Furthermore, when CAR T groups were compared to each other, CARs 1906 and 1940 stimulated the strongest reduction in MOLM-14 cellsLess, it is significantly higher than CARs 1936 and 1939. Thus, CARs 1906 and 1940 were most effective in controlling blood MOLM-14 levels, followed by CAR 1936 and CAR 1939.
Measurable levels of the inflammatory cytokines GM-CSF, IFN γ and IL-2 were detected in mice dosed with CAR T cells or UTD controls. Although the difference between the levels of these cytokines was not significant, plasma GM-CSF and IFN γ levels of construct 1906 tended to be higher, while IL-2 levels of CAR1906 and CAR constructs 1940 and 1936 tended to be elevated (fig. 11B). These results highlight the increased inflammatory cytokine secretion by activated CAR T cells. No significant differences were detected between experimental groups, probably because CAR T cells may have exceeded maximal activation at study day 19 (notably, tumor burden differences were detected as early as study day 14, fig. 10 a), however, CARs 1906 and 1940, which were most effective in tumor rejection, also tended to secrete higher levels of cytokines.
In summary, the high functionality of the novel fully human anti-CD 33 CAR construct LTG1906, as well as part of the functionality of constructs LTG1936 and LTG1939, was demonstrated in vitro and in vivo (table 2 below). It is envisaged that the function of constructs LTG1936 and LTG1939 could be further improved by redesigning the CAR spacer, linker or co-stimulatory domain to allow better access to the specific epitope it targets or to increase the level of CAR response to binding of tumor epitopes. Despite detectable surface expression and high cytokine secretion by flow cytometry, the VH-based anti-CD 33 CAR construct LTG1905 had low cytolytic effect. Despite high expression, ScFv-based CAR T constructs LTG1937 and LTG1938 were also inefficient at lysing target cell lines in vitro.
Example 3 improved functional properties of the CD33 CAR moiety can be achieved by altering the structure of anti-CD 33 CAR expressing fully human heavy chain-only or ScFv-based binding sequences
In this example, different structural configurations of anti-CD 33 CAR T cells derived from a novel fully human immunoglobulin heavy chain-only or scFv conjugate sequence are described.
When challenged with antigen-expressing tumor cells, it is hypothesized that CART cells secrete higher or lower levels of inflammatory cytokines, such as IL-2, IFN γ, TNF α, for example, by incorporating a single CD 28-derived vs CD137/4-1 BB-derived costimulatory domain (generation 2 CAR), a CAR structure lacking the costimulatory domain (generation 1 CAR), or incorporating multiple co-stimulatory domains in tandem (generation 3 CAR), in frame with an activation domain (e.g., CD3 ζ).
In some constructs, the incorporation of a novel hinge and transmembrane domain (e.g., a domain derived from the human TNFRSF19 sequence) may confer enhanced potency of the CAR in tumor cell killing and cytokine response.
Additionally, tumor antigens can be brought into better proximity to the CAR binding domain by varying the length and composition of the CAR hinge (also referred to as the linker domain), e.g., by replacing the CD8a derived linker domain with a variable length TNFRSSF19 derived domain or a domain derived from an immunoglobulin constant region and/or hinge, e.g., an IgG1 derived linker domain or an IgG4 derived linker domain incorporated into the CH2 and/or CH3 and/or hinge domain of an immunoglobulin molecule or modifications thereof. This is due to the fact that: the appropriate length and flexibility of the CAR hinge/linker domain is essential for optimal accessibility, binding to tumor antigens, and CAR T cell activation.
Furthermore, incorporation of a tag molecule in the CAR construct sequence expressed on the surface of the CAR T cell can be used 1) to identify CAR T cells during manufacture and in clinical applications by flow cytometry, 2) to sort/isolate CAR T cells during manufacture, 3) as a suicide tag to eliminate CAR T cells from the patient's body in the event of CAR-related toxicity, such as B-cell hypoplasia, cytokine release syndrome, or CAR-related neurotoxicity in response to anti-CD 19 CARs. To this end, the CAR construct sequence may comprise a truncated ectodomain and a transmembrane portion of a native transmembrane protein (e.g., HER1/EGFR, HER2/Neu/erbB-2, NGFR/LNGFR/CD271, CD19, CD20, or other protein). Mimotopes of these or other sequences may also be used. Removal of labeled CAR T cells from the circulation of the patient is achieved by administration of clinical grade antibodies with tag reactivity, such as antibodies targeting EGFR (cetuximab), HER2 (trastuzumab), CD20 (rituximab), or other proteins.
FIGS. 12A-12F show examples of choices of the CAR configurations described above, respectively. The described anti-CD 33 CAR construct was designed using a CD33 binding sequence derived from the immunoglobulin VH domain CD33_4, however, binder sequences in the form of ScFv can also be used.
Materials and methods:
(a) establishment of Chimeric Antigen Receptor (CAR) -expression vectors
The CAR antigen binding domain sequence is derived from a human anti-CD 33 ScFv or heavy chain variable fragment. The CAR T construct was generated by linking the binder sequence to the CD8a and transmembrane domain (UniProt sequence ID P01732, aa 138- "206) and then in-frame with the 4-1BB (CD137, aa 214-" 255, UniProt sequence ID Q07011) signaling domain and the CD3 zeta signaling domain (CD247, aa 52-163, reference sequence ID: NP-000725.1). For some constructs, the CD28 costimulatory sequence (UniProt ID: P10747, transmembrane domain, aa 153-179) was used instead of the 4-1BB costimulatory sequence. In some constructs, the CD8 ligation and/or transmembrane domain was replaced with a domain of various lengths derived from TNFRSF19 protein (UniProt ID: Q9NS 68). For some sequences, a truncated epidermal growth factor receptor (tEGFR) tag (UniProt ID: P00533, various sequences) was incorporated into the CAR construct via the 2A peptide to enable labeling of transduced cells in vitro, as well as to serve as a suicide switch for in vivo applications. CAR construct sequences were cloned into a third generation lentiviral plasmid backbone (Lentigen Technology inc., Gaithersburg, MD). Supernatants containing Lentiviral Vectors (LV) were generated by transient transfection of HEK 293T cells, the vectors were pelleted by centrifugation of the supernatants containing lentiviral vectors and stored at-80 ℃.
Table 2-expression and functional summary-anti-CD 33 CAR
Each of the applications and patents cited herein, and each document or reference cited in each of those applications and patents (including during the prosecution of each issued patent; "application citation"), and each of the PCT and foreign applications or patents corresponding to and/or claiming priority to any of those applications and patents, and each of the documents cited or referenced in each application citation, are hereby expressly incorporated herein by reference, and may be used in the practice of the present invention. More generally, several documents or references are cited herein, whether in the list of references preceding the claims or in the text itself; also, each of these documents or references ("herein cited references") and each document or reference cited in each herein cited reference (including any manufacturer specifications, guidelines, etc.) is hereby expressly incorporated by reference.
The foregoing description of some specific embodiments provides sufficient information so that others may, by applying current knowledge, readily modify or adapt for various applications such specific embodiments without departing from the generic concept, and, therefore, such adaptations and modifications should and are intended to be comprehended within the meaning and range of equivalents of the disclosed embodiments. It is to be understood that the phraseology or terminology employed herein is for the purpose of description and not of limitation. In the drawings and specification, there have been disclosed exemplary embodiments and, although specific terms may have been employed, they are unless otherwise stated used in a generic and descriptive sense only and not for purposes of limitation, the scope of the claims therefore not being so limited. Further, those of skill in the art will understand that certain steps of the methods discussed herein may be ordered in an alternative order or that steps may be combined. Therefore, it is intended that the appended claims not be limited to the particular embodiments disclosed herein. Those skilled in the art will recognize, or be able to ascertain using no more than routine experimentation, many equivalents to the embodiments of the invention described herein. Such equivalents are intended to be encompassed by the following claims.
Reference to sequence listing
This application contains the sequence listing, which is submitted electronically to the U.S. Patent and Trademark Office (United States Patent and trade Office) through a PDF file named "sequence listing," which is incorporated by reference.
Sequences of the present disclosure
The standard letter abbreviations for the nucleotide bases and the three letter codes for the amino acids defined in 37 c.f.r.1.822 are used to illustrate the nucleic acid and amino acid sequences listed below. Only one strand of each nucleic acid sequence is shown, but the complementary strand is understood to be included by any reference to the strand shown. In the attached sequence listing:
SEQ ID NO: nucleotide sequence of 1 CD 33-reactive immunoglobulin heavy chain variable domain (VH-2)
SEQ ID NO: amino acid sequence of 2 CD 33-reactive immunoglobulin heavy chain variable domain (VH-2)
SEQ ID NO: nucleotide sequence of 3 CD 33-reactive immunoglobulin heavy chain variable domain (VH-4)
SEQ ID NO: amino acid sequence of 4CD 33-reactive immunoglobulin heavy chain variable domain (VH-4)
SEQ ID NO: nucleotide sequence of 5 CD33 reactive ScFv9 binding domain
SEQ ID NO: amino acid sequence of 6 CD33 reactive ScFv9 binding domain
SEQ ID NO: nucleotide sequence of 7 CD33 reactive ScFv10 binding domain
SEQ ID NO: amino acid sequence of 8 CD33 reactive ScFv10 binding domain
SEQ ID NO: nucleotide sequence of 9 CD33 reactive ScFv12 binding domain
SEQ ID NO: amino acid sequence of 10 CD33 reactive ScFv12 binding domain
SEQ ID NO: nucleotide sequence of 11 CD33 reactive ScFv15 binding domain
SEQ ID NO: amino acid sequence of 12 CD33 reactive ScFv15 binding domain
SEQ ID NO: 13 leader/Signal peptide sequence
SEQ ID NO: 14 leader/Signal peptide sequence
SEQ ID NO: 15 LTG1905 _ (EF1a-VH-2 CD33-CD8 TM-41BB-CD3 ζ) nucleotide sequence
SEQ ID NO: 16 LTG1905 _ (EF1a-VH-2 CD33-CD8 TM-41BB-CD3 ζ)
SEQ ID NO: nucleotide sequence of 17 LTG1906 (EF1a-VH-4CD33-CD8 TM-41BB-CD3 zeta) nucleic acid sequence
SEQ ID NO: amino acid sequence of 18 LTG1906 (EF1a-VH-4CD33-CD8 TM-41BB-CD3 zeta)
SEQ ID NO: nucleotide sequence of 19 LTG1936 _ (EF1a _ ScFv9 CD33 CD8 TM-41BB-CD3 zeta CAR)
SEQ ID NO: 20 LTG1936 _ (EF1a _ ScFv9 CD33 CD8 TM-41BB-CD3 ζ)
SEQ ID NO: nucleotide sequence of 21 LTG1937 _ (EF1a _ ScFv10 CD33 CD8 TM-41BB-CD3 zeta CAR)
SEQ ID NO: 22 LTG1937 _ (EF1a _ ScFv10 CD33 CD8 TM-41BB-CD3 ζ)
SEQ ID NO: nucleotide sequence of 23 LTG1938 _ (EF1a _ ScFv12 CD33 CD8 TM-41BB-CD3 ζ)
SEQ ID NO: amino acid sequence of 24 LTG1938 _ (EF1a _ ScFv12 CD33 CD8 TM-41BB-CD3 ζ)
SEQ ID NO: nucleotide sequence of 25 LTG1939 _ (EF1a _ ScFv15 CD33 CD8 TM-41BB-CD3 ζ)
SEQ ID NO: 26 LTG1939 _ (EF1a _ ScFv15 CD33 CD8 TM-41BB-CD3 ζ)
SEQ ID NO: nucleotide sequence of transmembrane domain of 27 DNA CD8
SEQ ID NO: amino acid sequence of transmembrane domain of 28 CD8
SEQ ID NO: nucleotide sequence of 29 DNA CD8 hinge domain
SEQ ID NO: amino acid sequence of 30 CD8 hinge domain
SEQ ID NO: amino acid sequence of hinge region of amino acids 118 to 178 of 31 CD8 alpha (NCBI RefSeq: NP. sub. -001759.3)
SEQ ID NO: amino acid sequence of 32 human IgG CL sequence
SEQ ID NO: nucleotide sequence of 334-1 BB DNA signal transduction structural domain
SEQ ID NO: 344-1 BB Signal transduction Domain amino acid sequence
SEQ ID NO: nucleotide sequence of 35 CD3 zeta DNA signal transduction structural domain
SEQ ID NO: amino acid sequence of 36 CD3 zeta
SEQ ID NO: 37 Scvf cd19 nucleotide sequence
SEQ ID NO: 38 Scvf cd19 amino acid sequence
SEQ ID NO: nucleotide sequence of 39 GMCSF leader peptide
SEQ ID NO: amino acid sequence of 40 GMCSF leader peptide
SEQ ID NO: nucleotide sequence of 41 TNFRSF19 leader peptide
SEQ ID NO: amino acid sequence of 42 TNFRSF19 leader peptide
SEQ ID NO: nucleotide sequence of 43 CD8 alpha leader peptide
SEQ ID NO: amino acid sequence of 44 CD8 alpha leader peptide
SEQ ID NO: nucleotide sequence of 45 CD28 costimulatory domain
SEQ ID NO: amino acid sequence of 46 CD28 costimulatory domain
SEQ ID NO: nucleotide sequence of 47 CD3 zeta activation structural domain
SEQ ID NO: amino acid sequence of 48 CD3 zeta activation domain
SEQ ID NO: 49 nucleotide sequence of hinge and transmembrane domain of TNFRSF19 (transmembrane domain underlined)
SEQ ID NO: amino acid sequence of 50 TNFRSF19 hinge and transmembrane domain (transmembrane domain underlined)
SEQ ID NO: nucleotide sequence of 51 TNFRSF19 transmembrane domain
SEQ ID NO: amino acid sequence of 52 TNFRSF19 transmembrane domain
SEQ ID NO: nucleotide sequence of 53 TNFRSF19 hinge domain
SEQ ID NO: amino acid sequence of 54 TNFRSF19 hinge domain
SEQ ID NO: nucleotide sequence of 55 truncated TNFRSF19 hinge domain
SEQ ID NO: amino acid sequence of 56 truncated TNFRSF19 hinge domain
SEQ ID NO: nucleotide sequence of the hinge domain of CD8a fused to the transmembrane domain of TNFRSF19 (underlined transmembrane sequence)
SEQ ID NO: 58 amino acid sequence of the hinge domain of CD8a fused to the transmembrane domain of TNFRSF19 (underlined transmembrane sequence)
SEQ ID NO: nucleotide sequence of 59 CD28 costimulatory domain
SEQ ID NO: amino acid sequence of 60 CD28 costimulatory domain
SEQ ID NO: nucleotide sequence of 61 CD3 zeta form 2
SEQ ID NO: 62 CD3 zeta form 2 amino acid sequence
SEQ ID NO: nucleotide sequence of 63 furin P2A furin
SEQ ID NO: amino acid sequence of 64 furin P2A furin (furin sequence underlined)
SEQ ID NO: nucleotide sequence of 65 furin T2A
SEQ ID NO: 66 amino acid sequence of furin T2A (furin sequence underlined)
SEQ ID NO: 67 truncated EGFR (tEGFR) tag nucleotide sequence
SEQ ID NO: 68 truncated EGFR (tEGFR) tag amino acid sequence
SEQ ID NO: 69 LTG1927(EF1a-CD33_4-CD8 TM-CD28-CD3 ζ -cfrag)
SEQ ID NO: 70 LTG1927(EF1a-CD33_4-CD8 TM-CD28-CD3 ζ -cfrag)
SEQ ID NO: nucleotide sequence of nucleotide sequence 71 LTG _ D0033(Ef1a _ CD33_4VH TNFRSF 19H _ TM _ CD28z)
SEQ ID NO: amino acid sequence of nucleotide sequence of 72 LTG _ D0033(Ef1a _ CD33_4VH TNFRSF 19H _ TM _ CD28z)
SEQ ID NO: nucleotide sequence of 73 LTG _ D0034(Ef1a _ CD33_4VH TNFRSF 19H _ TM _4-1BBz) nucleotides
SEQ ID NO: amino acid sequence of 74 LTG _ D0034(Ef1a _ CD33_4VH TNFRSF 19H _ TM _4-1BBz)
SEQ ID NO: nucleotide sequence of 75 LTG _ D0015(Ef1a _ CD33_4VH CD8 BBz T2A tEGFR)
SEQ ID NO: amino acid sequence of 76 LTG _ D0015(Ef1a _ CD33_4VH CD8 BBz T2A tEGFR)
SEQ ID NO: nucleotide sequence of 77 LTG _ D0016(Ef1a CD33_4VH CD 828 z T2A tEGFR)
SEQ ID NO: amino acid sequence of 78 LTG _ D0016(Ef1a CD33_4VH CD 828 z T2A tEGFR)
SEQ ID NO: 79 nucleotide sequence of human IgG4 hinge
SEQ ID NO: amino acid sequence of 80 human IgG4 hinge
SEQ ID NO: nucleotide sequence of 81 human IgG4 CH2 domain
SEQ ID NO: amino acid sequence of 82 human IgG4 CH2 domain
SEQ ID NO: nucleotide sequence of 83 human IgG4 CH3 structural domain
SEQ ID NO: amino acid sequence of 84 human IgG4 CH3 domain
SEQ ID NO: nucleotide sequence of 85 human IgG4 hinge CH2 CH3 structural domain
SEQ ID NO: amino acid sequence of 86 human IgG4 hinge CH2 CH3 domain
SEQ ID NO: 87 LTG _ D0035(Ef1a _ CD33_4VH H CH2 CH3 IgG4_ CD8TM _ CD28z) by nucleotide sequence
SEQ ID NO: amino acid sequence of 88 LTG _ D0035(Ef1a _ CD33_4VH H CH2 CH3 IgG4_ CD8TM _ CD28z)
